Low seroprevalence of COVID-19 in Lao PDR, late 2020

Blood sample collection from participants in the community-based cohort, village office, Luangprabang province
Project Coordinator: Siriphone Virachith, Vilaysone Khounvisith, Antony Black
Other IPL laboratories: Virginie Pommelet, Elodie Calvez, Khamsing Vongphayloth, Vincent Lacoste, Somphavanh Somlor, Darouny Phonekeo, Paul T. Brey
Collaborating institutions: Lao Tropical Public Health Institute, Lao University of Health Sciences, National Centre for Laboratory and Epidemiology, Institut Pasteur, Paris, Luxembourg Institute of Health
Communications: report to collaborators, written report to International Pasteur Network, manuscript accepted for publication, online presentation to Pasteur COVID Scientific Meeting
Background
The Lao National COVID-19 task force was established in February 2020, approximately 3 months after the emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; the causative agent of COVID-19) in Wuhan, China. In the middle of March 2020, the task force implemented restrictions such as school closure (until May 2020) and a lockdown was implemented from the 20th of March until the 3rd of May. Domestic flights were canceled until May 15, and a restriction on most international flights was started.
From January 2020, testing for COVID-19, as recommended by WHO guidelines, was conducted on nasopharyngeal and oropharyngeal swabs using real-time reverse transcription polymerase chain reaction (RT-PCR). This testing was done on suspected cases – those with symptoms including fever and at least one of the following: cough, runny nose, sore throat, shortness of breath, or difficulty to breath – and their contacts. Travelers into and out of Lao PDR were also tested by the same technique and a 14-day quarantine was imposed on all arrivals.
Although the first case of COVID-19 in Lao PDR was confirmed early – on March 24, 2020 – there were less than 40 SARS-CoV-2 positive confirmed cases in total in 2020 and no recorded COVID-19-related deaths. This low number contrasted with those of several southeast Asian countries and was among the lowest proportionally worldwide.
The low number of confirmed COVID-19 cases in 2020 could largely be due to the strict control measures set in place by the Lao Government. Another reason could be the relatively low population density limiting the spread of the virus or the young age structure of the population; 51% are under 24 years old and less than 7% over 60. This young population may allow mild or asymptomatic infections (approximately 80% of COVID-19 cases) to go undetected. This is particularly relevant in the context of countries, such as Lao PDR, where routine disease surveillance is challenging.
Healthcare workers are a particular risk group who may come into contact with COVID-19 patients. Importantly, the seroprevalence of anti-SARS-CoV-2 antibodies within healthcare settings can offer insight into the effectiveness of infection prevention and control measures. Another potential risk group for infection is individuals in close contact with wildlife including bats, one of the natural reservoirs of coronaviruses, possibly including SARS-CoV-2 or its progenitor. The large diversity of bat species in Lao PDR and the geographical closeness of the Hubei province in China where SARSCoV- 2 was first detected suggest that such viruses could naturally circulate in Lao PDR.
In this context, the seroprevalence of antibodies against SARS-CoV-2 before vaccine introduction is a crucial indicator of virus exposure and can guide prevention measures. Recent studies have demonstrated a heterogeneous anti-SARS-CoV-2 seroprevalence depending on the location and serological studies can indicate the circulation of SARS-CoV-2 in the absence of detection by routine surveillance.
Thus, the aim of this study was to determine the seroprevalence of anti-SARS-CoV-2 antibodies in the general population, healthcare workers, and individuals with close contact with bats/wildlife in Lao PDR.
Methods
Population selection and recruitment
In this study, three cross-sectional seroprevalence surveys were conducted in parallel from August to September 2020: a population-based survey and two sub-surveys focusing on two high-risk groups: healthcare workers and guano-collectors, wildlife traders and people in close contacts with bats.
For the population-based survey and the healthcare workers survey, five provinces were selected: Vientiane Capital, two provinces in the North-Luang-Prabang, Oudomxay and two provinces in the South -Savannakhet and Champassak (Figure 1).
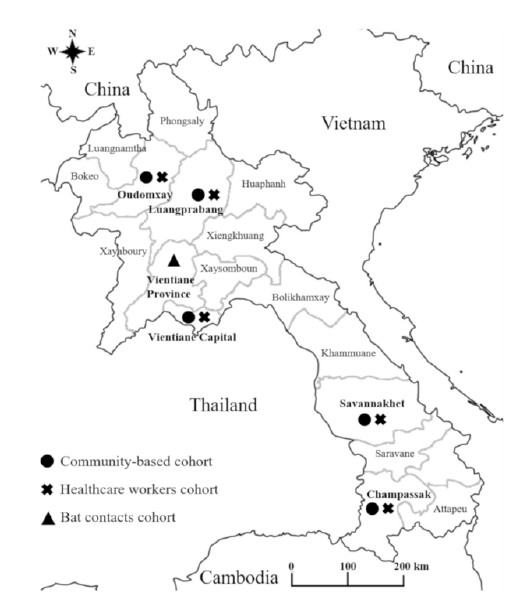
Figure 1. Map of Lao PDR showing study locations.
Participants of the population-based survey were selected using a multistage cluster sampling design to select households in the five provinces. In each province, districts were randomly selected and considered as strata. In each district, villages were then randomly selected using the probability-proportional-to-size (PPS) sampling method using official lists of villages based on the population data from the 2015 census. A fixed number of households were then randomly selected in each village and in each household; all inhabitants aged five and above were invited to participate. In Vientiane Capital, four districts were randomly selected, then nine villages were selected using the PPS method and six households were randomly selected. In the four other provinces, three districts were selected per province; six villages and five households of each village were selected (see sample size calculation).
In Vientiane Capital, the survey focusing on healthcare workers was conducted in four central hospitals and in two district hospitals.
In the four other provinces, only healthcare workers working in the provincial hospitals were included. All staff assigned to dedicated COVID-19 teams were invited to participate -including clinical and non-clinical staff (e.g administrative staff, drivers, cleaners, etc). In central and provincial hospitals, nurses, doctors and lab-technicians working in emergency departments (ER), outpatient departments (OPD), intensive care units (ICU), infectious disease departments, inpatient departments (IPD) and pediatric departments were randomly selected maintaining the nurses to doctors ratio in each department. In the two district hospitals, staff working in the OPD and ER were randomly selected.
For the wildlife contacts, four villages in Feung District, Vientiane province, were visited in September 2020. The villages were selected as they are locations where the profession of bat guano collecting – for selling as fertilizer – is common. Villagers who had contact with bats or other wildlife were informed about the study by the head of their village and invited to participate.
5mL of whole blood was collected into dry collection tubes and allowed to clot. Serum was separated by centrifugation and stored at 4°C for a maximum of seven days until storage at -80°C.
Sample size calculation
For the high-risk groups, we aimed to recruit around 900 healthcare workers in the three regions and 100 bat/ wildlife contacts in Vientiane Province. In order to establish the cut-off values and validate the anti-N and anti-S ELISAs, 265 pre-COVID-19 samples were tested. These samples were collected as part of a separate hospital-based zero study in the South of Lao PDR in 2018 (ethics approval number NECHR018/2017). In addition, serum from 15 confirmed SARS-CoV-2 patients from Lao PDR, collected between four and nine weeks after diagnosis and ten longitudinal samples from one patient (diagnosed in France and living in Lao PDR) were used after consent was obtained.
Antibody detection
SARS-CoV-2-specific anti-nucleocapsid (N) and anti-spike (S) antibodies were detected by ELISA. IgM/ IgG rapid tests were done according to the manufacturer’s instructions. These tests are reported by the manufacturer to have sensitivity and specificity of 100% and approximately 99%, respectively.
Ethics approval
The study protocol was approved by all participating institutes and by the Lao National Ethics Committee for Health Research (NECHR) (Ref #052/2020). Oral and written informed consent was obtained from people aged 15 years and older. Parental consent was taken for children aged between 5 and 11 years, and assent from children aged between 12 and 14 years in addition to parental consent, before the survey.
Results
Participants
A total of 3173 participants were recruited between the 12th of August and the 25th of September 2020. This consisted of participants from the general population (n=2433; mean age 42.6years (range 5-55) and healthcare workers (n=666; mean age 36.8 years (range 20-65)) from two Northern, one Central and two Southern provinces (Table 1 and Figure 1). Seventy-four serum samples were collected from bat/wildlife contacts; 12 bat guano collectors, five wildlife animal vendors and 57 bat contacts, catchers, or bat guano collectors’ families in Vientiane Province (mean age 43.5years (range 17-86)).
1593 individuals were unavailable for the study due to reasons such as “working” or “at school” and were therefore replaced by other randomized participants from the same location. Only two healthcare workers and six people from the community-based cohort refused to participate in the study due to fear of needles and unwillingness to answer questions.
Table 1. Participant demographics
*Missing country of travel for 4 participants
**China, Vietnam, Korea
Anti-N and anti-S antibody serology
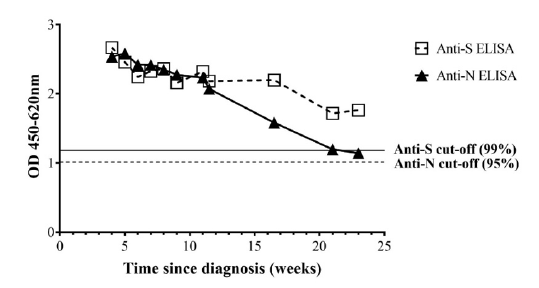
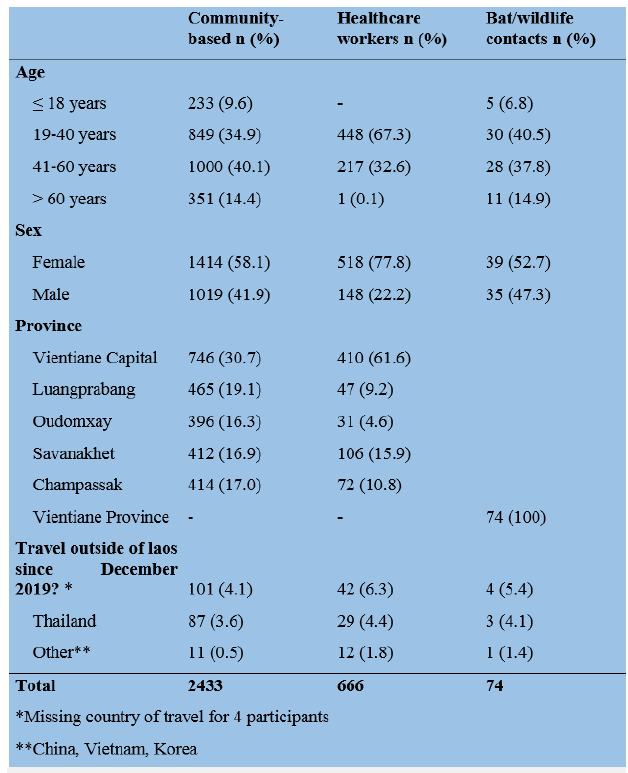
Figure 2. Longitudinal anti-N and anti-S antibody serology. Data represent the mean of duplicate results from a COVID-19 positive individual (diagnosed in France, end of August 2020).
Cut-offs of 95% and 99% were set for defining anti-N and S antibody seropositivity, using pre-COVID-19 samples taken from individuals in the South of Lao PDR in 2018. Thus, 14/265 (5.3% [3.1-8.7%]) pre-COVID-19 samples were positive for anti-N antibodies. Three pre- COVID-19 samples were positive for anti-S antibodies (1.1% [0.3-3.5%]). No pre-COVID-19 samples were double-positive for anti-N and anti-S antibodies and 3 double-negative samples (1.1%) were anti-SARS-CoV-2 IgM positive (1.1%) and one IgG positive (0.4%) by rapid test. Longitudinal samples from the French confirmed cases with mild symptoms showed double-positive N and S antibody seropositivity and were rapid test positive until at least 21 weeks post-diagnosis despite a decline in ELISA OD (Figure 2). Samples from confirmed COVID-19 cases identified by the national COVID-19 surveillance in Lao PDR (n=15) were all double-positive for anti-N- and S-antibodies and rapid test positive (Figure 3).
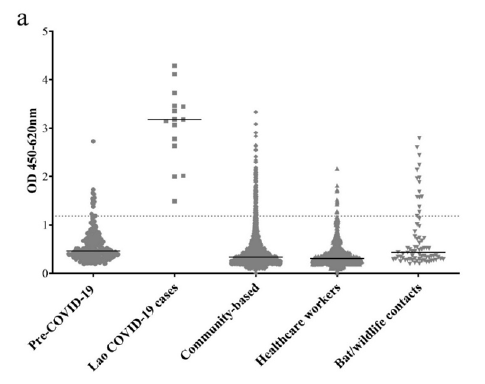
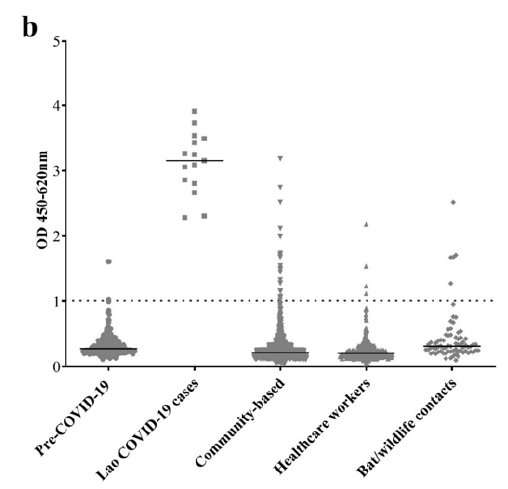
Figure 3. a. Anti-N antibodies b. Anti-S antibodies. Data show the average of duplicate OD values for each sample. The dotted line represents the OD of 95% cut-off for anti-N antibodies and 99% cut-off for anti-S antibodies, established from the pre-COVID-19 samples. The solid lines represent the median OD.
In the participant samples from 2020, anti-N antibodies were detected in only 131/2433 (5.4% [4.5-6.3%]) of the general population, 13/666 (2.0% [1.3-3.3%]) of the healthcare workers but 15/74 (20.3% [12.6-31.0%]) of the bat/wildlife contacts.
Only 3/159 (1.9% [0.6-5.7%]) of the anti-N antibody positive samples were positive by rapid test (one IgM single positive and two IgM/IgG double positive). These samples were all anti-S antibody negative and therefore they were not considered as true “COVID-19 cases”. Due to limited reagents, anti-S antibody ELISAs were done on a smaller selection of participants (n=1417), including all anti-N antibody positive participants and all bat/ wildlife contacts plus a randomly selected sample from the general population and healthcare workers. Anti-S antibodies were detected in only 19/1061 (1.8% [1.2- 2.8%]) of the general population, 4/282 (1.4% [0.3-3.7%]) of the healthcare workers and 5/74 (6.8% [2.8-15.3%]) of the bat/wildlife contacts. Only two out of all 2020 participant samples (2/3173; 0.1%) were double-positive for both anti-N and anti-S antibodies (Figure 4). These two samples were from the general population and were negative by anti-SARS-CoV-2 IgM/IgG rapid test and therefore also considered unlikely to be true “COVID-19 cases”.
Only one of the anti-S antibody positive samples from the 2020 participants was rapid test positive (IgG). This participant was a bat/wildlife contact (anti-N antibody negative) aged 74 years. He had worked previously as a guano collector in caves. Two members of his family tested negative for anti-N and anti-S antibodies although his daughter had traveled to Thailand five months previously.
Within the general population, anti-N antibody positive status increased with age from 3.9% before 18 years to 8.8% above 61 years (p<0.0001, using score test for trend of odds). No other parameters were associated with anti-N or S antibody status in any cohort.
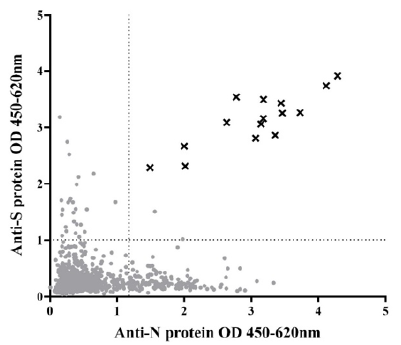
Figure 4. Relationship between anti-N and anti-S antibody amounts. Points show mean OD of individual samples from the general population, healthcare workers, and bat/wildlife contacts. Crosses represent the mean OD of 15 confirmed SARS-CoV-2 cases, identified by the Lao national surveillance. Dotted lines represent 95% cut-off value for anti-N antibodies and 99% cut-off for anti-S antibodies.
Discussion
In this study, performed in Lao PDR from August until September 2020, the seroprevalence of anti-SARS-CoV-2 antibodies in the general population and healthcare workers was extremely low. These data likely reflect the low incidence of COVID-19 within the country and are in agreement with the few confirmed cases to date and low reported rates of hospitalization of patients with respiratory illnesses in Lao PDR.
Why did Lao PDR remain largely free of COVID-19 in 2020, in contrast to many other countries? The answer is likely a combination of several factors. Firstly, the Government of Lao PDR implemented a robust control of visitors from outside the country, starting in March 2020. This included greatly restricting the number of commercial flights, and the requirement of all visitors to have proof of a negative SARS-CoV-2 RT-PCR test within the previous 72 hours, a negative test upon arrival, and to undertake a 14-day quarantine upon arrival. Even before such measures, Lao PDR had a relatively small number of international arrivals and, additionally, the land border point-of-entries are mostly connected to low-density areas of neighboring countries. In addition, the rapid and decisive response of the Government of Lao PDR and other countries in the Lower Mekong region perhaps reflects a greater preparedness for pandemic outbreaks, born out of the experience with SARS-CoV-1 in 2002-2003 and several avian influenza outbreaks in recent years.
An association between low population density and reduced COVID-19 incidence has been shown in some studies but not others. Thus, even though the population is not evenly distributed throughout the country, the low population density in Lao PDR -approximately 32 people per km2 – may have played some role in limiting the spread of COVID-19 to date. In addition, as younger people are more likely to be asymptomatic, the young age structure of the population may have reduced the number of symptomatic cases and disease-associated mortality. The lack of a mass-transit system could be another factor.
We cannot discount that some cultural or societal factors played a role, such as a low number of people traveling within the country. Physical contact may be lower in Lao PDR, for example, shaking hands is not common and hand-holding in public is rare, while wearing facemasks is often practiced. Lastly, it has been speculated that climate may have some role in the spread of SARCoV- 2, with the spread being limited in warmer and more humid environments. However, this is unlikely to have made a significant impact in Lao PDR, given the high rates of infection in countries with similar climates.
N and S proteins from SARS-CoV-2 have been shown to be highly immunogenic, with anti-S antibodies being more specific. In our study, pre-COVID-19 controls from 2018 had anti-N and anti-S antibody seroprevalence of 5.3% and 1.1%, respectively, with none seropositive for both although three (1.1%) were positive by IgM rapid test. Seroprevalence studies in France observed similar pre-COVID-19 levels of anti-SARS-CoV-2, likely representing cross-reaction with non-SARSCoV- 2 coronaviruses. In the 2020 study participants, we found that there were only 159/3173 (5.0%) seropositive for anti-N antibodies and only 28/1417 (2.0%) were seropositive for anti-S antibodies. Only two participants (0.1%) were double-seropositive for anti-S and -N antibodies. These participants were negative by IgM/ IgG rapid test and likely represent false positives as the prevalence was similar to the pre-COVID-19 controls. Some of the “single-positives” may reflect true crossreactivity with other unknown or seasonal alpha- and beta- coronaviruses such as HKU1, NL63, OC43 and 229E. Notably, it is thought that most pre-existing crossreactive antibodies do not confer protection against SARS-CoV-2 (38). Although a prior infection with SARSCoV- 1, the causative agent of SARS, may confer crossreactivity to SARS-CoV-2 due to neutralizing activity of antibodies against the highly homologous Receptor Binding Domain, such instances are probably insignificant in Lao PDR. It is nevertheless possible that exposure to other coronaviruses occurs in Lao PDR given the frequent trade in bushmeat and low biosafety awareness.
Indeed, it has been shown that bats and rodents from Lao PDR and bordering countries can be infected with a diverse array of alpha- and beta- coronaviruses including SARS-CoV-2–like viruses. The participants in our study who had frequent contact with bats or other wildlife had high anti-N antibody seroprevalence. Also, one bat/ wildlife contact whose daughter had been to Thailand five months previously was anti-S antibody positive, anti-N antibody negative and rapid test (IgG) positive. This could be due to exposure to coronaviruses from wildlife although we have no control group from the same location, and anti-S antibodies are thought to be less cross-reactive than anti-N antibodies. Neutralization assays were not performed on these samples and it remains possible that there was a localized COVID-19 outbreak in this population. Therefore, in addition to coronavirus detection and typing among the bats and other wildlife populations, these particular populations deserve further studies.
Anti-SARS-CoV-2 antibodies in mild cases are thought to be lost rapidly – up to 20% of such cases in neighboring Thailand were shown to be seronegative within two weeks after the onset of symptoms. It is, therefore, possible that some of the participants in the current study were infected with SARS-CoV-2 and did not seroconvert or had lost antibodies by the time of the study. However, similar to other studies, longitudinal samples from one patient who was infected in late August 2020 and presented only mild symptoms were seropositive for anti-N antibody until at least week 21 after diagnosis and longer for anti-S antibodies.
The main limitation of this study was that only five of the 18 Lao provinces were purposively selected. However, these provinces were selected due to a perceived high risk of SARS-CoV-2 introduction (international flight arrivals into Luang Prabang and Vientiane Capital, large numbers of Chinese migrant workers in Oudomxay, and migrant workers returning to Lao PDR from Thailand in Champasak and Savannakhet). Nevertheless, it is possible that we missed areas where SARS-CoV-2 virus entered e.g. from neighboring countries in the North.
Other limitations included the non-representative nature of the age structure of the sampled population. Lastly, clarification regarding the cross-reactive nature of the few anti-N and anti-S antibodies detected in participants and pre-COVID-19 samples could be determined by neutralization assays, which were not available to us at the time of the study. Despite these caveats, we believe that it is highly unlikely that the results would change in any meaningful way given the sample size and the three different tests used.
In summary, our data indicate that Lao PDR remained largely free of COVID-19, at least until late 2020. The Government of Lao PDR should be commended on the swift and decisive action taken to reduce the risk of SARSCoV- 2 introductions into the country. Nevertheless, Lao PDR remains at risk of virus introduction, either from neighboring countries or further afield. The borders cannot remain closed indefinitely and therefore other measures need to be strengthened such as active surveillance, vaccination of at-risk groups and vaccination status checks at points of entry. With the rapid development and opening up of the country, such as the imminent launch of the high-speed rail system connecting China, Lao PDR and Thailand, this is as pertinent as ever. Lastly, the high seroprevalence of anti-N antibodies in bat/wildlife contacts in Lao PDR is a stark reminder that the threat of emergence of future pandemics is real and that steps need to be taken to mitigate and prepare for them.