Project for Development of Innovative Research Technique in Genetic Epidemiology of Malaria and Other Parasitic Diseases in Lao PDR for Containment of Their Expanding Endemicity
Project leader: Dr. Shigeyuki Kano
Member of staff: Moritoshi Iwagami, Phonepadith Xangsayarath, Phonepadith Khattignavong, Sengdeuane Keomalaphet, Pheovaly Soundala, Lavy Lorphachan, and other visiting scientists and students
Background
Malaria, Schistosomiasis (Schistosoma mekongi) and Opisthorchiasis (Opisthorchis viverrini) have tremendous health burden on the people in Lao PDR. Although significant reductions in malaria transmission have been reported due to the large-scale insecticide-treated bed nets (ITNs) distribution through the Global Fund to Fight AIDS, Tuberculosis and Malaria, strategies based on the scientific evidence have not been developed to deal with the genetic variation in parasites and vectors population, and drug resistant malaria. Recently, artemisinin resistant malaria was reported in Attapeu province in 2014 (Ashley et al., 2014). Therefore, it is necessary to survey other provinces especially in the southern part of the country to monitor and contain the spread of drug resistant malaria. Lao Ministry of Health and WHO set a goal to eliminate malaria by 2030. To achieve this goal, we have to understand real malaria situation including drug resistant malaria and to develop elimination strategies.
Since Schistosomiasis (S. mekongi) and Opisthorchiasis (O. viverrini) are localized to Lao PDR and surrounding countries, they are recognized as neglected tropical diseases. Nevertheless, the prevalence of Opisthorchiasis is estimated as high as 15-54% in Lao PDR. Little information on the molecular/genetic epidemiology of the Opisthorchiasis is available to develop effective measures for prevention and diagnosis of the diseases.
The Government of Lao PDR requested Japan International Cooperation Agency (JICA) to establish the Lao-Japan Joint laboratory within Institut Pasteur du Laos (IPL) for conducting highly technological research on human malaria parasites: Plasmodium falciparum, P. vivax, and monkey malaria parasite: P. knowlesi, and human trematodiasis: S. mekongi and O. viverrini. The joint research will concentrate on genetic epidemiological studies to detect and control of the emergence and dissemination of these parasitic diseases. The Project also contributes to the capacity development of researchers and technicians in Lao PDR through training of field and Lab work, seminar and career development.
In order to carry out this project, the IPL collaborates with National Center for Global Health and Medicine (NCGM), Tokyo, Japan, Center of Malariology, Parasitology and Entomology (CMPE), National Institute of Public Health (NIOPH), and other Departments, Ministry of Health, Lao PDR.
Objective
Objectives of this project are (1) to develop more convenient and accurate methods (PCR methods, LAMP methods, etc.) for diagnosis of the diseases, (2) to monitor temporal and spatial epidemiological situations of pathogens and vectors of the diseases, (3) to analyze mechanisms of emergence and expansion of the drug resistant malaria, especially, artemisinin resistance, and (4) to analyze glucose-6-phosphate dehydrogenase (G6PD) activity of Lao population for evaluation of possible usage of primaquine (Howes et al., 2013), utilizing molecular biological techniques.
Based on the scientific evidence obtained by this project, health education for the people will be strengthened and endemicity of the diseases will be monitored together with the local Lao Ministry of Health. Research results will also be utilized in government services for sustainable development of Lao PDR.
Study period of the project
Five years (May 2014 to April 2019)
Study sites of the project
Malaria:
Savannakhet province, Saravane province, Sekong province, Attapeu province, Champasak province, Khammouane province, Phong Sali province, Luang Prabang province
Schistosomiasis (S. mekongi):
Khong district and Mounlapamok district, Champasak province
Ethical clearance
The SATREPS project was approved by the National Ethics Committee for Health Research in the National Institute of Public Health (NIOPH), Ministry of Health, Lao PDR in 2014, 2015 (extend every one year).
Activities and Results in October 2014 to October 2015
We conducted 7 field surveys on parasitic diseases and 3 training courses of parasitic diseases diagnoses for medical lab technicians at IPL and 5 training courses in 5 southern provinces (Savannakhet, Saravane, Sekong, Champasak, and Attapeu) since we published IPL Activities Report 2014. This activities report summarized our activities and results of the SATREPS project in Parasitology lab from October 2014 to October 2015.
All field surveys were conducted with collaboration with Center of Malariology, Parasitology and Entomology (CMPE), Provincial Health Office, and District Health Office, Ministry of Health, Lao PDR. All the training courses at IPL were also conducted with collaboration with CMPE and all the training courses at provinces were conducted with collaboration with CMPE and Provincial Health Office.
Field surveys on Malaria, Schistosomiasis and Opisthorchiasis
+ Schistosomiasis and Opisthorchiasis Survey, Khong district, Champasak province on 8th-12th December 2014
+ Malaria Survey of foreign migrant population, Thapangtong district, Savannakhet province on 26th February-5th March 2015
+ Schistosomiasis and Opisthorchiasis Survey, Khong district, Champasak province on 20th-25th April 2015
+ Malaria Survey, Xaysetha district, Phouvong district, Sanamxay district, Attapeu province on 9th-16th May 2015
+ Schistosomiasis and Opisthorchiasis Survey, Mounlapamok district, Champasak province on 17th-23rd May 2015
+ Opisthorchiasis Survey, Yommalath district, Khammouane province on 16th-26th August 2015
+ Opisthorchiasis Survey, Yommalath district, Khammouane province on 20th-30th September 2015
Malaria field surveys
Written informed consent was obtained from all the participants prior to the interview and blood collection for malaria diagnosis. Three malaria diagnostic methods: microscopy, rapid diagnostic test (RDT: Malaria Ag Pf/Pv, Standard Diagnostics, Inc. Republic of Korea) and DNA diagnostic test (PCR method) were used for detecting malaria parasites, malaria parasites antigen and malaria parasites DNA, respectively.
Malaria Survey for foreign migrant population, Thapangtong district, Savannakhet province on 26th February – 5th March 2015
This survey was conducted in collaboration with Dr. Tiengkham POMGVONGSA, Director of Malaria Section, Savannakhet Provincial Health Office, and a team of University of the Ryukyus leaded by Professor Jun KOBAYASHI, Associate Professor Daisuke NONAKA, who are members of the SATREPS project. Seventy-seven foreign migrant workers participated in this malaria survey: 64 Vietnamese, 7 Chinese and 6 Thai. Four out of 77 participants refused blood examination (malaria RDT & microscopy) and blood collection on a filter paper. Malaria RDT was conducted on site of the survey, while microscopy was conducted at Malaria Station in Savannakhet province, and PCR analysis was conducted at IPL. All the participants were malaria negative by all the diagnostic methods.
Malaria Survey, Xaysetha district, Phouvong district, Sanamxay district, Attapeu province on 9th-16th May 2015
A master course student, Dr. Sengdeuane KEOMALAPHET, from Institut Francophone de Medecine Tropicale (IFMT) joined this survey and now she is a member of Parasitology lab at IPL. A total of 719 villagers in Attapeu province participated in this malaria survey. Table 1 shows summary of the survey.
Table 1. Summary of Malaria survey in Attapeu province in May 2015
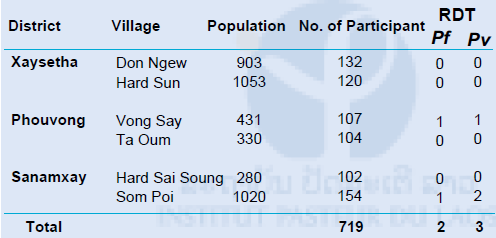
RDT: Rapid Diagnostic Test (Malaria Ag Pf / Pv, Standard Diagnostics, Inc. Republic of Korea), Pf : Plasmodium falciparum, Pv : P. vivax
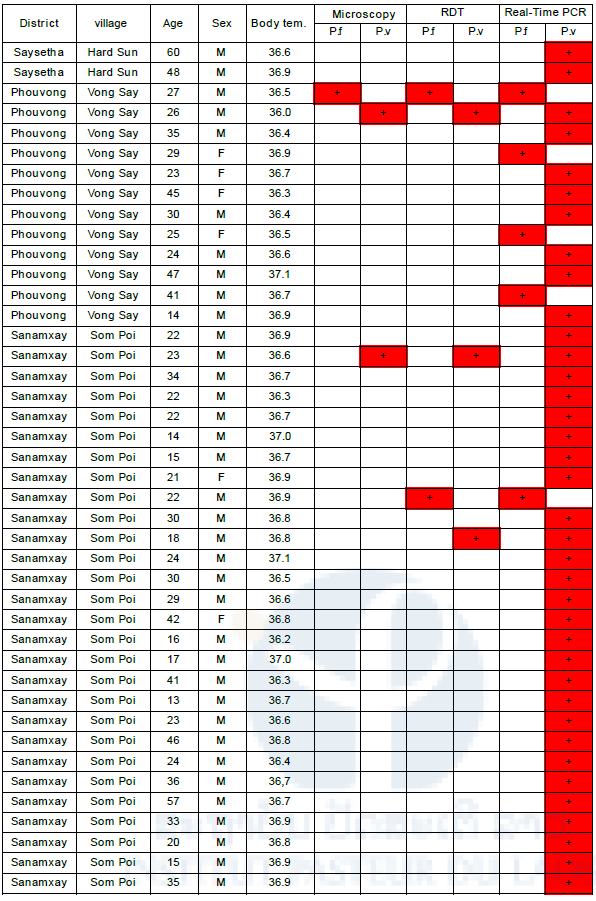
RDT was conducted on site of the survey, and microscopy and PCR analysis were conducted at IPL. When the participants were diagnosed as malaria by RDT in the survey, Health Center or District Hospital provided antimalarial drugs (Coartem: artemether and lumefantrine) to them. A total of 381 blood samples (120 from Hard Sun, 107 from Vong Say and 154 from Som Poi villages) were analyzed by the 3 methods (Table 2). The remaining 338 blood samples are under analysis at IPL. Genomic DNA was extracted from the filter papers using a QIAamp DNA Mini Kit® (Qiagen, Valencia, CA, USA). Nested real-time PCR was used to detect malaria parasites DNA. First, universal human malaria parasites primer set was used, and second, species specific primer sets (P. falciparum and P. vivax) were used for malaria parasites DNA detection. Partial cytochrome b gene in mitochondrial genome of P. falciparum and P. vivax was used as a target of the PCR analysis. A total of 339 samples were malaria DNA negative, while 42 samples were malaria DNA positive by real-time PCR methods. Table 2 shows detail of 42 malaria DNA positive cases in this study.
All the 42 malaria parasites DNA positive cases were asymptomatic. Average body temperature of them was
36.7oC and no one was higher than 37.5oC. Average age of them was 29 years old. Number of male and female were 36 and 6, respectively (P < 0.05). A manuscript of these data is in preparation for publication.
Table 2. Summary of malaria positive cases by 3 diagnostic tests
Discussion of malaria survey in Attapeu province in May 2015
The analyses showed that all of the positive cases were asymptomatic malaria parasites carriers (parasite reservoir, or hidden malaria) and that adult male was a high-risk population in the areas. According to WHO World Malaria Report 2015, 62% of malaria cases in Laos were P. falciparum and 38% of them were P. vivax. On the contrary, our survey showed that P. vivax is a dominant species (88.1%: 37/42) in the study areas. Our survey was conducted in May (dry season). This might be influenced malaria transmission dynamics in the endemic area. Generally, malaria season is rainy season because mosquito density is high in rainy season, although this pattern is getting unclear in Laos. P. vivax has a dormant stage called “hypnozoite” in human liver cells that causes relapse of vivax malaria months, or even a year later. Only primaquine can treat hypnozoite but this antimalarial drug cannot be used for people who have G6PD deficiency. G6PD deficiency is a genetic disorder and if G6PD deficiency people take primaquine, acute hemolytic anemia is liable to occur. In Laos, this drug is not officially used because few information about G6PD deficiency among the population is available so far and G6PD test kit is not available in the country yet, except Luang Prabang, Savannakhet and Champasak provinces where a pilot primaquine treatment for vivax malaria patients was conducted in 2015 by Lao Ministry of Health with support of WHO. Therefore, P. vivax has a potential to be a dominant species during dry season in Attapeu province.
Further survey, especially in rainy season is needed to understand malaria transmission in the study areas. Moreover, to understand real malaria transmission status in the country, wide range of malaria sample collection in 5 southern provinces (Savannakhet, Saravane, Sekong, Champasak, and Attapeu) has been conducted by the SATREPS project with the collaboration of Provincial Health offices, District Hospitals and Health Centers.
Schistosomiasis and Opisthorchiasis Surveys
Written informed consent was obtained from all the participants prior to the interview and stool collection for diagnosis of Schistosomiasis and Opisthorchiasis.
Schistosomiasis and Opisthorchiasis Survey, Khong district, Champasak province on 8th-12th December 2014
This survey was conducted at Donetharn Secondary School, Donlong Island in Khong district. It was one week before mass drug administration (MDA) of praziquantel. One hundred and ninety-two students participated in this survey. Stool examination by microscopy was conducted by 2 methods: Kato-Katz (KK) method and Formalin-Detergent (FD) method for detecting the parasite eggs in the stool samples either on site or at IPL. The results of the stool examination were shown in Table 3 (KK method) and 4 (FD method). By KK method, 25.0% of students (48/192) were O. viverrini positive, while by FD method, 25.7% of students (49/191) were O. viverrini positive including mixed infection with O. viverrini and other parasites. S. mekongi egg was not observed in this study.
Table 3. Results of KK method in Khong district, Champasak province in December 2014
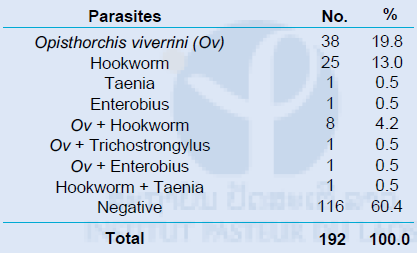
Table 4. Results of FD method in Khong district, Champasak province in December 2014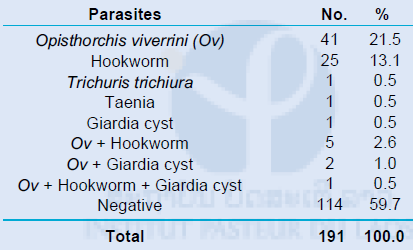
DNA diagnostic method (LAMP method) was also conducted using the 110 stool samples at Tokyo Medical and Dental University, Japan. Only 7 out of 110 samples were Opisthorchis viverrini DNA positive by LAMP method.
A total of 2,559 freshwater snails (resembling Neotricula aperta) was collected at Donglong Island near the school. Infection rate of S. mekongi of the snails was examined by microscopy and by LAMP method targeting cox1 gene of mitochondrial genome of S. mekongi, but all of the snails were negative for S. mekongi.
Schistosomiasis and Opisthorchiasis Survey, Khong district, Champasak province on 20th-25th April 2015
This survey was conducted at Donetharn Secondary School, Donlong Island in Khong district 4 months after MDA of praziquantel. One hundred and fifty-two students participated in this survey. They are same population at the same school in the previous survey in December 2014. However, the sample size of this survey (152) was smaller than that of the previous survey (192) because some of the students were taking Lao new year holidays (middle of April). Stool examination by microscopy was conducted by Kato-Katz (KK) method (triplicate) for detecting parasite eggs in the stool samples either on site or at IPL. The results of stool examination were shown in Table 5. In this survey, 21.1% of students (32/152) were O. viverrini positive including mixed infection with O. viverrini and other parasites, while 1.3% of students (2/152) were S. mekongi positive. They are mixed infection with O. viverrini.
Table 5. Results of KK method (Triplicate) in Khong district, Champasak province in April 2015
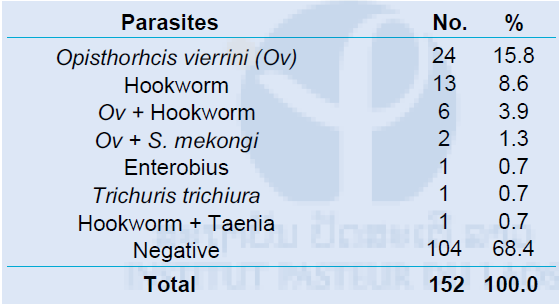
DNA diagnostic method (LAMP method) was also conducted using the 152 stool samples at Tokyo Medical and Dental University, Japan. ITS1 region of rRNA gene of the parasites nuclear genome was used as a target gene for LAMP method. 13.8% of samples (21/152) were Opisthorchis viverrini DNA positive, while 0.7% of samples (1/152) were S. mekongi DNA positive by LAMP method. This result suggested that sensitivity of LAMP method was lower than that of microscopy (KK method) or that the O. viverrini egg might be an O. viverrini-like egg, “minute intestinal fluke” (Sayasone et al., 2009). Further analysis is needed to elucidate this issue. A manuscript of these data is in preparation for publication.
A total of 1,975 freshwater snails (resembling Neotricula aperta) was collected at Donglong Island near the school. Infection rate of S. mekongi in the snails was examined by microscopy and LAMP method targeting cox1 gene of mitochondrial genome of S. mekongi, but all of the snails were negative for S. mekongi. Species of the collected snails was identified by PCR and DNA sequencing in Tokyo Medical and Dental University, Japan, as Neotricula aperta gamma strain which is reported as a host of S. mekongi. The molecular phylogenetic tree of the snails was shown in Figure 1.
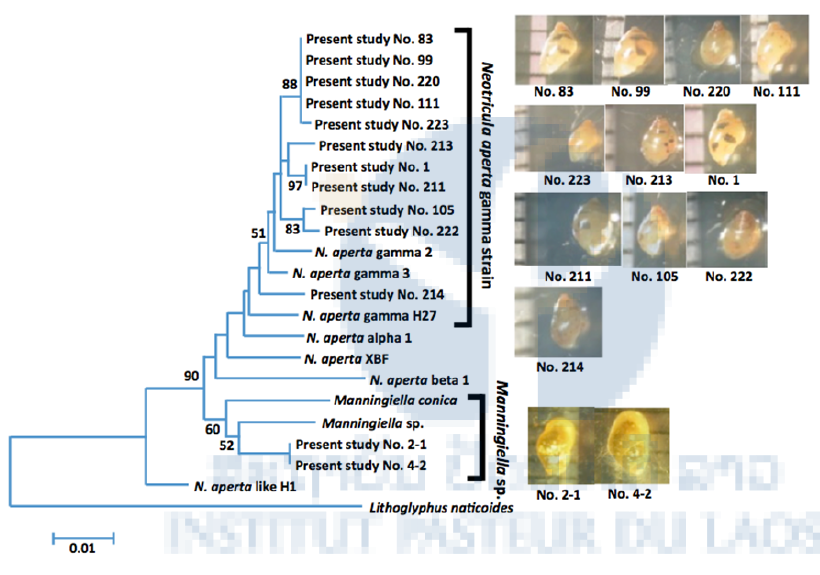
Figure 1. Molecular phylogenetic tree of Neotricula aperta gamma strain collected in Donglong Island in Champasak province in 2015
Schistosomiasis and Opisthorchiasis Survey, Mounlapamok district, Champasak province on 17th-23rd May 2015
This survey was conducted at 2 villages: Nady and Sanva in Mounlapamok district 3 months after MDA of praziquantel. A total of 325 villagers participated in this survey. Stool examination by microscopy was conducted by Kato-Katz (KK) method (triplicate) for detecting parasite eggs in the stool samples either on site or at IPL. The results of stool examination were shown in Table 6. In this survey, 69.5% of villagers (226/325) were O. viverrini positive, while 0.3% of villager (1/325) was S. mekongi positive, including mixed infection. LAMP analysis for detecting S. mekongi and O. viverrini is now being conducted at Tokyo Medical and Dental University, Japan. A manuscript of these data is in preparation for publication.
Table 6. Results of KK method (Triplicate) in Mounlapamok district, Champasak province in May 2015
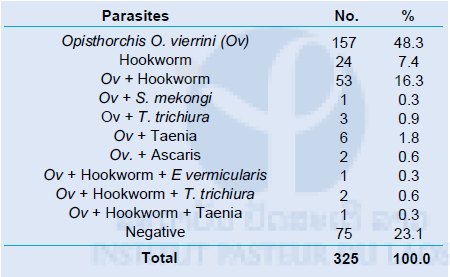
E. vermicularis: Enterobius vermicularis, T. trichiura: Trichuris trichiura
Opisthorchiasis Survey, Yommalath district, Khammouane province on 16th-26th August 2015
Lao Ministry of Health has been conducting MDA of praziquantel in combination with health education/promotion for villagers in the endemic provinces of Opisthorchiasis for control of the disease. However, infection rate of Opisthorchiasis has been still high in the endemic areas. To find a breakthrough for the control, we attempted to find out positive deviance in the villagers. Positive deviance approach is to identify good practices that are linked to good outcomes, such as preventing malnutrition of children, and infectious diseases.
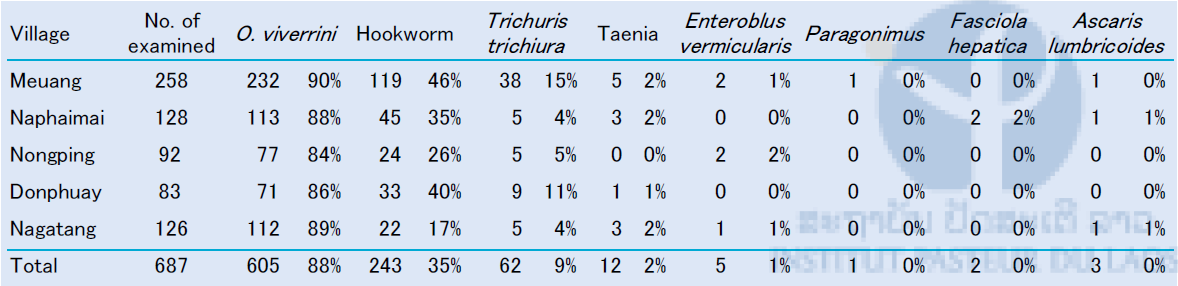
This survey was conducted at 5 villages (Meuang, Na Phaimai, Nong Ping, Don Phuay, Nagatang) in Yommalath district 8 months after MDA of praziquantel. Yommalath district is known to be one of the high Opisthorchiasis endemic areas in Laos. A pair of 348 mothers and one of their children in the villages participated in this survey (total 696 villagers). Detail questionnaire survey was conducted with mothers, and stool samples were collected from both mothers and one of their children. Consequently, stool samples were collected from 687 villagers. Nine samples were not collected in this survey. Stool examination by microscopy was conducted by Kato-Katz (KK) method (triplicate) for detecting parasite eggs either on site or at IPL. The result of stool examination was shown in Table 7. A manuscript of these data is in preparation for publication.
Table 7. Results of KK method in Yommalath district, Khammouane province in August 2015
Opisthorchiasis Survey, Yommalath district, Khammouane province on 20th-30th September 2015
This survey was conducted at 5 villages (Meuang, Na Phaimai, Nong Ping, Don Phuay, Nagatang) in Yommalath district 9 months after MDA of praziquantel. This was the second survey to find out positive deviance that was associated to prevent O. viverrini (Ov) infection. We visited 44 households (families) to observe their kitchen, cooking, and washing utensils and interviewed their eating habit as well. Those 44 households were selected based on the results of the first Opisthorchiasis survey in Yommalath district in August 2015. They were 10 Ov negative families (both mother -/child -), 34 Ov half-positive families (mother + /child -), and 1 Ov full-positive family (both mother +/child . In this survey, we also collected stool samples from all family members and examined by Kato-Katz (KK) method (triplicate) for detecting parasite eggs either on site or at IPL.
We found that Ov negative families tended to clean their kitchen and utensils consciously compared to Ov positive families. For example, cutting boards at Ov negative families were clean, and in fact, such families had more than 1 cutting boards: one for cutting fish or meat and the other for cutting vegetables (Figure 2 & 3). This finding may be a positive deviance for preventing Ov infection. The data are now being analyzed at the University of Tokyo.

Figure 2. Cutting board in a kitchen at Ov negative family. The surface of the board was clean.

Figure 3. Cutting board in a kitchen at Ov positive family. Many fish scales were on the surface of the board.
Discussion of Opisthorchiasis survey in Champasak and Khammouane provinces in 2014 and 2015
Lao Ministry of Health has been conducting MDA of praziquantel and health education/promotion for control of trematode infections, especially Opisthorchiasis in several provinces and Schistosomiasis in Champasak province. However, the infection rate of Opisthorchiasis has still been high in several endemic areas. This can be explained by low coverage of the MDA and re-infection of O. viverrini by eating raw or insufficiently cooked freshwater fish that is contaminated with O. viverrini metacercariae. Low coverage of praziquantel MDA may be due to its severe side effects, such as, severe epilepsy, rash, nausea, headache, dizziness, abdominal pain, or diarrhea. Thus, there are strict inclusion/exclusion criteria of praziquantel MDA made by Lao Ministry of Health. According to the criteria, people with chronic disease, epilepsy, central nervous system problem, pregnancy and lactating woman will be excluded. This is the limitation of praziquantel MDA. Therefore, health education is crucial to make people aware of the need to stop eating raw or undercooked fish and to use latrine in their villages.
Training courses of parasitic disease diagnosis for medical lab technicians at IPL and provinces
Summary of the training courses at IPL and provinces
The objective of this training course is to increase knowledge and improve skills of effective diagnosis of malaria and other parasitic diseases for medical lab technicians at provincial and district levels in 5 southern provinces (Savannakhet, Saravane, Sekong, Champasak and Attapeu), that are now reported to be high malaria endemic provinces in Laos. Medical lab technicians or staff members from Malaria Station in provincial capital and district, District Hospitals and Health Centers attended the training courses. Target districts were selected based on Annual Parasite Incidence (AP
I: number of malaria case/1,000 population/year) reported by CMPE in 2013. We conducted 3 training courses at IPL and 5 training courses at the provinces. Detail of participants of the training courses is shown in Table 8.
Table 8. Number of participants from the 5 southern provinces
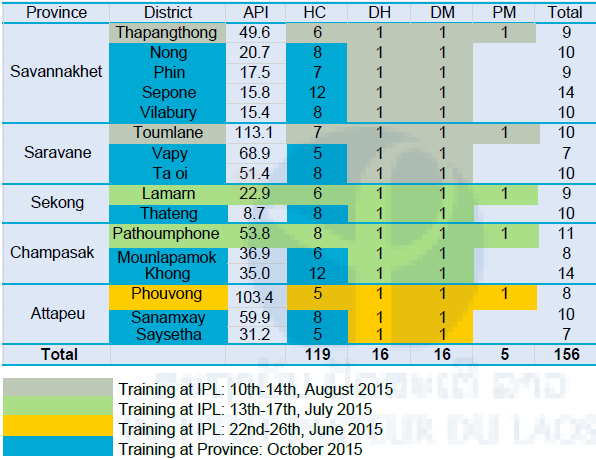
API: Annual Parasite Incidence (No. of malaria case/1,000 population), HC: Health Center, DH: District Hospital, DM: District Malaria Station, PM: Provincial Malaria Station.
Training at IPL:
+ Attapeu (12) on 22nd-26th June 2015
+ Sekong (11) and Champasak (15) on 13th-17th July 2015
+ Savannakhet (17) and Saravane (14) on 10th-14th August 2015
Training at provinces:
+ Savannakhet (35) on 19th-20th October 2015
+ Champasak (18) on 22nd-23rd October 2015
+ Saravane (13) on 26th-27th October 2015
+ Sekong (8) on 28th-29th October 2015
+ Attapeu (13) on 31st October 2015
Numbers in parentheses represent number of participants of the training.
Blood sample collection from malaria suspected patients at Hospitals and Health Centers in the 5 southern provinces
We provided filter papers (FTATM Classic Card, GE Healthcare Life Sciences, WhatmanTM, UK) for collecting blood samples from malaria suspected patients to the medical lab technicians (participants) of the training courses. The first sample collection was conducted at the 5 southern provinces on October 2015 from the participants who attended our training courses at IPL on June, July and August 2015. A total of 4,441 blood samples were collected from malaria suspected patients (both positive and negative by microscopy or RDT). About 13 % of the samples (587/4,441) were malaria positive by microscopy or RDT (Table 9). In Laos, standard diagnostic method for malaria is microscopy at hospitals level, while RDT is used at community level where microscope is not available.
Malaria DNA analysis is now being conducted using those filter paper blood samples. First, malaria parasite species will be identified by the nested real-time PCR. Second, mutation of drug resistant genes, such as K13, pfcrt, will be examined using P. falciparum positive samples. Third, population genetic analyses will be conducted using highly polymorphic DNA markers of malaria parasites, such as microsatellite DNA loci to understand transmission dynamics of malaria in Laos (Iwagami et al., 2012 & 2013).
Table 9. Number of filter papers collected from malaria suspected patients in the 5 southern provinces in October 2015
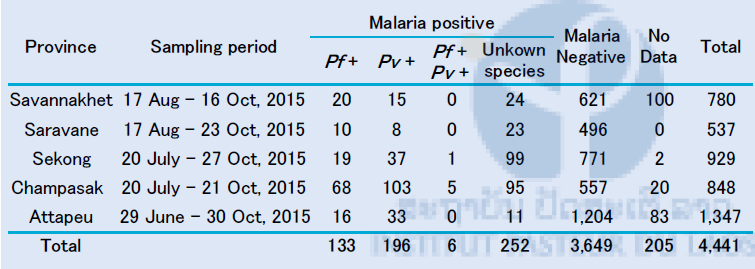
RDT: Rapid Diagnostic Test (Malaria Ag Pf / Pv, Standard Diagnostics, Inc. Republic of Korea)
Partners
+ Center of Malariology, Parasitology and Entomology (CMPE), Ministry of Health, Vientiane Capital, Lao PDR
+ National Institute of Public Health (NIOPH), Ministry of Health, Vientiane Capital, Lao PDR
+ Department of Communicable Diseases Control (DCDC), Ministry of Health, Vientiane Capital, Lao PDR
+ Department of Training and Research (DTR), Ministry of Health, Vientiane Capital, Lao PDR
+ Department of Hygiene and Health Promotion (DHHP), Ministry of Health, Vientiane Capital, Lao PDR
+ National Center for Global Health and Medicine (NCGM), Tokyo, Japan
+ Department of Community and Global Health, School of International Health, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan
+ Department of Global Health, Graduate School of Health Sciences, University of the Ryukyus, Okinawa, Japan
+ Department of Molecular and Cellular Parasitology, Juntendo University School of Medicine, Tokyo, Japan
+ Section of Environmental Parasitology, Department of International Health Development, Division of Public Health, Graduate School, Tokyo Medical and Dental University, Tokyo, Japan
Scientific communications
Publication:
Didier Ménard, et al;KARMA Investigators (Author: Shigeyuki Kano, Contributors: Moritoshi Iwagami, Paul Brey). A Worldwide Map of Plasmodium falciparum Artemisinin Resistance. New England Journal of Medicine, 2016, 374(25): 2453-2464
Oral presentations:
Moritoshi Iwagami, Phonepadith Khattignavong, Pheovaly Soundala, Lavy Lorphachan, Sengdeuane Keomalaphet, Mixay Phommakhod, Bouasy Hongvanthong, Paul T. Brey, Shigeyuki Kano. Current Malaria Situation in Lao PDR based on DNA analysis. The 9th National Health Research Forum, Vientiane Capital, Lao PDR, October 13th-14th, 2015.
Phonepadith Khattignavong, Enn Sayavong, Pheovaly Soundala, Masami Nakatsu, Satoshi Nakamura, S. Maithaviphet, C. Keomanivong, K. Silavong, B. Phommavongsa, K. Keokenchanh, T. Keobouachanh, H. Keomanila, S. Chanthavongsa, Bouasy Hongvanthong, Moritoshi Iwagami, Shigeyuki Kano, Paul T. Brey. Detection of Plasmodium falciparum and P. vivax in Anopheles mosquitoes in Lao PDR by DNA analysis. The 9th National Health Research Forum, Vientiane Capital, Lao PDR, October 13th-14th, 2015.
Masamine Jimba, Hitomi Araki, Ong I Ken, Moritoshi Iwagami, Bouasy Hongvanthong, Paul T. Brey, Shigeyuki Kano. Positive Deviance Approach for Overcoming NTDs. The 9th National Health Research Forum, Vientiane Capital, Lao PDR, October 13th -14th, 2015
Tiengkham Pongvongsa, Panom Phongmany, Bouasy Hongvanhthong, Daisuke Nonaka, Jun Kobayashi, Moji Kazuhiko, Shigeyuki Kano. Malaria Situation and Challenges in Savannakhet Province. The 9th National Health Research Forum, Vientiane Capital, Lao PDR, October 13th -14th, 2015
Takashi Kumagai, Moritoshi Iwagami, Masafumi Yamabe, Phonepadith Khattignavong, Lavy Lorphacan, Pheovaly Soundala, Bouasy Hongvanthong, Nobuo Ohta, Paul T. Brey, Shigeyuki Kano. The Evaluation of the Molecular Diagnosis using LAMP method against the Parasitic trematoda in Champasak Province, southern Lao PDR. The 9th National Health Research Forum, Vientiane Capital, Lao PDR, October 13th -14th, 2015
Moritoshi Iwagami, Phonepadith Khattignavong, Pheovaly Soundala, Lavy Lorphachan, Sengdeuan Keomalaphet, Mixay Phommakhod, Bouasy Hongvanthong, Paul T. Brey, Shigeyuki Kano. Genetic Epidemiology of Malaria in Lao PDR by SATREPS Project. The 56th Annual Meeting of the Japanese Society of Tropical Medicine. Osaka, Japan, December 4th-6th, 2015
Poster presentation:
Kumagai Takashi et al. Schistosoma mekongi and Opisthorchis viverrini infection in Khong district in Lao PDR. The 9th Annual Meeting of Helminth Research, Iwate, Japan, July 17th-18th, 2015
Shigeyuki Kano. Development of Innovative Research Technique in Genetic Epidemiology of Malaria and Other Parasitic Diseases in Lao PDR fro Containment of Their Expanding Endemicity. The 30th Annual Meeting of Japan Society of International Health, Kanazawa, Japan, November 21st, 2015
Kei Mikita, Masami Nakatsu, Akihiko Doi, Noppadon Tangpukdee, Srivicha Krudsood, Shigeyuki Kano. Polymorphisms in Plasmodium falciparum K13-propeller from Than-Myanmar border in 1996-1997. Joint International Tropical Medicine Meeting 2015, Bangkok, December 2nd-4th, 2015
Moritoshi Iwagami, Phonepadith Khattignavong, Pheovaly Soundala, Lavy Lorphachan, Sengdeuane Keomalaphet, Mixay Phommakhod, Bouasy Hongvanthong, Paul T. Brey, Shigeyuki Kano. Current Malaria Situation in Lao PDR based on DNA analysis by SATREPS Project. Joint International Tropical Medicine Meeting 2015, Bangkok, Thailand, December 2nd-4th, 2015
Acknowledgement / Funding
We wish to thank Dr. Bouasy HONGVANTHONG, Director of CMPE, Ministry of Health, Lao PDR, and Project director of SATREPS for his kind support of this project. We thank Dr. Tiengkham POMGVONGSA, Director of Malaria Station, Savannakhet Provincial Health Department, Lao PDR. We also thank the staff of the CMPE, the NIOPH, Provincial Health Offices, Provincial Hospitals, District Hospitals and Health Centers, Lao Ministry of Health for supporting our field surveys and training courses.
This work is supported by SATREPS (Science and Technology Research Partnership for Sustainable Development) project from Japan International Cooperation Agency (JICA) and Japan Agency for Medical Research and Development (AMED).

References
1. Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. New England Journal of Medicine, 371: 411-423, 2014.
2. Howes RE, Dewi M, Piel FB, Monteiro WM, Battle KE, Messina JP, et al. Spatial distribution of G6PD deficiency variants across malaria-endemic regions. Malaria Journal, 12: 418, 2013.
3. World Health Organization. World Malaria Report 2015, Geneva, Switzerland
4. Sayasone S, Vonghajack Y, Vanmany M, Rasphone O, Tesana S, Utzinger J, et al. Diversity of human intestinal helminthiasis in Lao PDR. Transactions of the Royal Society of Tropical Medicine and Hygiene, 103: 247-254, 2009.
5. Iwagami M, Fukumoto M, Hwang SY, Kim SH, Kho WG, Kano S. Population structure and transmission dynamics of Plasmodium vivax in the Republic of Korea based on microsatellite DNA analysis. PLoS Neglected Tropical Diseases, 6: e1592, 2012.
6. Iwagami M, Hwang SY, Kim SH, Park SJ, Lee GY, Matsumoto-Takahashi EL, Kho WG, Kano S. Microsatellite DNA analysis revealed a drastic genetic change of Plasmodium vivax population in the Republic of Korea during 2002 and 2003. PLoS Neglected Tropical Diseases, 7: e2522, 2013.