Risk of vector-borne diseases in relation to rubber plantations in Côte d’Ivoire as compared to Lao PDR.
Project coordinator: Dr. Paul Brey and Pr. Mireille Dosso Global coordinator: Julie-Anne Tangena
Member of staff: Dr. Bernard Kouadio Allali, Dr. Ibrahima Zanakoungo Coulibaly, Issouf Traoré, Dr. Phoutmany Thammavong and Somsanith Choneserath
Funded by the Michelin Corporate Foundation

Background:
The ECOMORE project has given great insight into the risks of vector-borne disease transmission in rubber plantations of northern Lao PDR. The importance of rubber plantation habitats for the dynamics for vector-borne diseases is an issue that also needs to be considered for other areas in the world where rubber plantation habitats are common. As far as we are aware no studies have been conducted on the risk of vector-borne diseases in rubber plantations outside South-east Asia (SEA), except of an onchocerciasis risk study among residents of a rubber plantation in Liberia [53, 54]. With growing evidence of increased vector-borne disease risk in rubber plantations of SEA, it is of interest to identify the vector-borne disease dynamics in rubber plantation areas established in Africa and South America. This is especially pressing in sub-Saharan Africa where vector-borne diseases such as malaria and yellow fever still result in a high number of morbidity and mortality [55, 56]. .
Rationale:
Côte d’Ivoire has the largest area of rubber plantation in the whole of Africa. We anticipate that the changes in the environment to rubber cultivation is resulting in an altered risk from vector-borne diseases for the local population with increased risk of exposure to vector mosquitoes for the rubber workers and their families; predominantly malaria and yellow fever, but also arboviral diseases such as dengue and chikungunya. This study will provide an opportunity to further develop the entomological department at Institut Pasteur de Côte d’Ivoire whilst deepening our understanding of the vector ecology in rubber plantations in West Africa. Furthermore this data will be combined with data collected in a similar fashion in Lao PDR to write a comprehensive document about the vector-borne disease risks for rubber workers. It is envisaged that this project will allow us to advise different governmental and health organizations how to decrease vector-borne disease incidence in rubber plantation areas where active transmission of vector-borne diseases already occurs. For this purpose we will also be comparing commercially available personal protection methods in the field both for their protectiveness from mosquitoes and acceptance by the local population. This study will be of relevance to public health workers, governments and those working in the rubber industries of Côte d’Ivoire, other countries in West Africa and SEA. The goal of this study is to assess the potential risk of vector-borne disease infections occurring in and around rubber plantations.
The study objectives are:
1. Determine the risk of mosquito-borne diseases like malaria, yellow fever, dengue and chikungunya arising in rubber plantations compared to surrounding villages
2. Understand when and where rubber plantation workers are exposed to the vector mosquitoes
3. Provide advice on how to decrease exposure of rubber plantation workers, their families and the local population to vector-borne diseases
4. Understand the differences and similarities between Laos and Côte d’Ivoire in vector-borne disease risk in rubber plantation
Update until October 2016:
During the last year the Yersin team has spent considerable time in the field, both in Côte d’Ivoire and in Lao PDR. In Côte d’Ivoire the team has continued its successful adult mosquito data collection in the field which was started in December 2015. In Lao PDR during two months of intense fieldwork, data has been collected on the protectiveness of different personal protection methods. In the following paragraphs we will go into detail on our activities in both countries for this project.
Côte d’Ivoire:
Since the start of the fieldwork in December 2015 adult mosquito collection in Côte d’Ivoire have been conducted successfully for 10 months in the three study sites, each consisting of four different habitats (mature rubber plantation, immature rubber plantation, village surrounded by rubber plantations and villages without plantations in the area). Two more months of adult mosquito collection are planned until November 2016, after which data can be fully analysed. Until July 2016 (8 months) a total of 5,451 female mosquitoes and 1,030 male mosquitoes have been collected using the human-baited double net (HDN) trap. The preliminary data highlights the high density of mosquitoes collected in the mature rubber plantations (n=1,117), immature rubber plantations (n=1,684) and villages away from the plantations (n=1,979). Low numbers have been collected in the villages surrounded by rubber plantations (n=671). This data gives a first insight into the importance of rubber plantations as mosquito habitats. However this does not result in information regarding the risk of vector-borne diseases, with not all mosquitoes able to transmit diseases. In the paragraph below we focus on the three most important and abundant vector mosquito species collected in the field.
We have summarized the data of the first eight months of collection for the important malaria, yellow fever and lymphatic filariasis vectors to give insight into the data collected. The most abundant malaria vector Anopheles gambiae s.l. was collected a total of 61 times. The malaria vector seems more prevalent in the villages than in the rubber plantations with more than half of the samples collected from the villages surrounded by rubber plantations. The vector was mostly active from 22.00 to 02.00 O’clock when villagers were asleep. Contrary to the malaria vector, the density of the yellow fever and dengue vector Aedes aegypti was highest in mature and immature rubber plantations where 95% of the total 1,402 Aedes aegypti samples were collected. The vector was active throughout the day with a peak from 16.00 to 18.00 O’clock. A total of 2,031 Culex quinquefasciatus mosquitoes have been collected during the first eight months of collection. This important vector of lymphatic filariasis was generally collected in high numbers from the villages away from the rubber plantations. Peak collection period was from 19.00 to 22.00 O’clock when villagers were preparing to go to sleep. The preliminary results presented here give a first insight into the data. The vector presence and behaviour will be analysed at the end of 2016 when data is complete.
Apart from the adult mosquito identification we are also analysing the collected vector samples for parity rate of the ovaries, which gives an indication of the survival rate of the mosquitoes. Using this survival rate we can identify the longevity of the mosquitoes, with long living vector mosquitoes resulting in more effective disease vectors. After collection of adult mosquitoes has been completed in December 2016 we will use both the adult mosquito prevalence and survival rate for calculations of the basic reproductive number (R0) which gives an indication of the number of infections one disease case can generate on average during the course of its infectious period in a certain habitat. If the basic reproduction number is for example two, this entails that one infective human case can result in two new infective human cases. The higher the basic reproductive number in a habitat, the higher the risk the disease establishes itself in the habitat.
Rapid rural appraisals have been conducted in November 2015 to assess the knowledge among villagers regarding vector-borne diseases and to extract general behavioural patterns of the villagers and rubber workers. Currently we are in the process of conducting tri-monthly surveys in the field to collect additional data on the behaviour of the local villagers and rubber workers in the different habitats throughout the year. Using the results from both the rapid rural appraisals and surveys we will identify several common behavioural patterns. The combination of the human behaviour data and entomological data will enable us to identify risky behaviour for vector-borne diseases. This information will be used to inform the government and local population on when and where villagers and rubber workers are exposed to vector-borne diseases, risky behaviour and how to mitigate these risks.
The knowledge on how to mitigate vector-borne disease risk alone is not enough to decrease vector-borne disease incidence. It is important to identify how we can communicate our recommendations to the local populations. To identify the best methods with which we can reach the local population, we will conduct several focus group discussion in the study area. We have identified social scientist students from the local university to help conduct these discussions and analyse the data. We are currently in the process of writing the standard Operating Procedure (SOP) which will be implemented in the field in 2017.
Next year we plan to collect data on the breeding sites of the important vector species identified during the adult mosquito survey. We are currently updating the SOP of the larval survey. The survey will be conducted throughout 2017 in the same habitats where adult surveys are currently taking place. The identification of the main waterbodies where mosquitoes breed, will be used to design vector control strategies and and write recommendations on how to decrease vector numbers in the area.
Lao PDR:
In July 2016 we received the approval from all ethical committees (Institut Pasteur Paris, Durham University and the Lao government) for our personal-protection methods comparison study. We started our fieldwork at the end of July 2016 in northern Lao PDR. For 8 weeks we worked in the field to collect adult mosquitoes using five treatments and two untreated controls (Table 1). Collections were conducted using human landing catches for 6 consecutive hours in villages at night and in forested areas during the day. A total of 14 comparison days and 28 comparison nights were done. A total of 32 participants were involved, whom all received a long lasting insecticide-treated net and relevant health insurances. Furthermore participants were paid for their work collecting mosquitoes. All collected mosquitoes have already been identified to species. We are now in the process of entering all data in digital files for analysis. During the next trimester focus will be on cleaning the data and analysing the results for recommendations.
Table 1: The five treatments and two controls of the comparison study
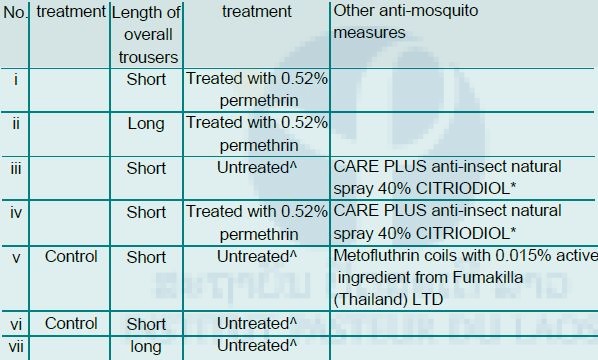
All untreated clothing has gone through the same procedure (i.e. factory dipping) but without the active ingredient for fair comparison.* was applied once to exposed skin during the six hour collection period. Repellent was applied by the responsible (i.e. Julie-Anne Tangena) at a rate of four dose (sprays) per limb to decrease variation of application among participants
Apart from understanding which method protects people from mosquito bites, it is important to understand the user friendliness of the products. In the beginning of September 2016 we conducted 28 surveys among the participants of the comparison study to identify their preference. We not only asked them which method protected them from mosquito bites, but also which method was most comfortable and easy to wear. We also asked them about their monthly investment in personal protection methods to understand the availably finances in each household for the purchase of personal protection methods. With this information we hope to assess the acceptability of the personal protection methods in our study area. We are currently analysing this data.
In August 2016 we conducted 12 focus group discussions with the help of two social scientist students from Vientiane University. Focus group discussions were conducted with young boys (< 20 years), young girls (< 20 years), male adults (20-35 years), female adults (20-35 years), old male adults (> 35 years) and old female adults (> 35 years). In small groups the local villagers were asked to share their experience and knowledge of mosquitoes and mosquito-borne diseases. Furthermore we asked them about the current methods used by the government to communicate information to the local villagers (eg. meetings, posters, radio spots, t-shirts) and which methods they preferred. The focus group discussions are currently being transcribed and translated. Data will be analysed for trends.
Communication:
Every three months the Yersin team has been writing a newsletter on the activities of this project. This newsletter is written for distribution by the Michelin Corporate Foundation to inform people outside the scientific world on the project. This two page newsletter includes a roadmap, updates from the field and preliminary results. We will continue writing newsletters every three months until the end of the project.
A representative of the Michelin Corporate Foundation, Mister Phillipe Legrez, visited the Ivorian and Lao team in Côte d’Ivoire from the 27th to the 29th of January 2016 to discuss the project achievements so far and to see the Yersin activities in the field. The HDN trap was clarified and presented in the field. Additionally in each of the three study villages a small meeting was held with the village head, village elderly and study participants to talk about the project and its impact on the village. Furthermore the district health centre was visited to understand the impact of mosquito-borne diseases on people living in the area and how they are helped. All in all, the visit of Mr. Legrez was a great opportunity for the project team to show the progress of the project and a great opportunity to discuss the project in detail to ensure the goals and objectives of the project are met.
The research director from the Ministry of Research Côte d’Ivoire, director of the National Institute of Hygiene Côte d’Ivoire, representative of the National Center of Agricultural Research (CNRA), Ivorian entomologists and other representatives from the research field were present to witness the official opening. The research director from the Ministry of Research, the director of Institut Pasteur de Côte d’Ivoire Pr. Dosso and Mr. Legrez gave a small talk on the impact of the Yersin project. A balafong band provided music during the ceremony. After the ceremony the ribbon of the building was cut and everyone received a short tour of the building. On the whole the inauguration ceremony provided us with a great opportunity to highlight the Yersin project to the research and government community of Côte d’Ivoire.
Future activities:
In 2017 the focus of the Yersin project will be on both the analysis of data collected in 2016 and conducting additional field work. The data analysis will consist of entering the data, cleaning the data and using statistical analysis to investigate the data. The data will be used to write scientific papers and the conclusions from these papers will be communicated as recommendations to the local populations and health offices in the region. The field work in 2017 will mainly take place in Côte d’Ivoire with both a larval survey and social study planned for next year.
Reference:
1. Golding N, Wilson A, Moyes C, Cano J, Pigott D, Velayudhan R, Brooker S, Smith D, Hay S, Lindsay S: Integrating vector control across diseases. BMC Medicine 2015, 13:249.
2. McMichael AJ, Patz J, Kovats RS: Impacts of global environmental change on future health and health care in tropical countries. Br Med Bull 1998, 54:475-488.
3. Foley JA, DeFries R, Asner GP, Barford C, Bonan G, Carpenter SR, Chapin FS, Coe MT, Daily GC, Gibbs HK, et al: Global consequences of land use. Science 2005, 309:570-574.
4. Patz JA, Olson SH, Uejio CK, Gibbs HK: Disease emergence from global climate and land use change. Med Clin North Am 2008, 92:1473-1491.
5. Norris D: Mosquito-borne diseases as a consequence of land use change. EcoHealth 2004, 1:19-24.
6. Parham PE, Waldock J, Christophides GK, Hemming D, Agusto F, Evans KJ, Fefferman N, Gaff H, Gumel A, LaDeau S, et al: Climate, environmental and socio-economic change: weighing up the balance in vector-borne disease transmission. Phil Trans R Soc B 2015, 370:1665.
7. Githeko AK, Lindsay SW, Confalonieri UE, Patz JA: Climate change and vector-borne diseases: a regional analysis. Bull World Health Organ 2000, 78:1136-1147.
8. Millenium Ecosystem Assessment: Chapter 14: Human health: ecosystem regulation of infectious diseases. In Ecosystems and Human Well-being: Current State and Trends. Washington: MEA; 2005.
9. Yasuoka J, Levins R: Impact of deforestation and agricultural development on anopheline ecology and malaria epidemiology. Am J Trop Med Hyg 2007, 76:450-460.
10. Manivong V: Economic potential for smallholder rubber production in Northern Laos. University of Queensland, School of Natural and Rural Systems Management; 2007.
11. Cairns M: Voices from the forest: integrating indigenous knowledge into sustainable upland farming, Chapter 49. 2007: 603-605
12. National Agriculture and Forestry Research Institute: Review of rubber plantations. In Rubber plantation information book (National Agriculture and Forestry Research Institute, Ministry of agriculture and forestry eds.). Vientiane: Ministry of Agriculture and Forestry, NAFRI; 2016.
13. Dondero TJJ, Menon VV: Clinical epidemiology of filariasis due to Brugia malayi on a rubber estate in west Malaysia. Southeast Asian J Trop Med Public Health 1972, 3:355-365.
14. Singh J, Tham AS: Case history on malaria vector control through the application of environmental management in Malaysia. vol. 154776. Geneva: WHO; 1988.
15. Singhasivanon P, Thimasarn K, Yimsamran S, Linthicum K, Nualchawee K, Dawreang D, Kongrod S, Premmanisakul N, Maneeboonyang W, Salazar N: Malaria in tree crop plantations in south-eastern and western provinces of Thailand. Southeast Asian Journal of Tropical Medicine and Public Health 1999, 30:399-404.
16. Yasuoka J, Levins R: Impact of deforestation and agricultural development on anopheline ecology and malaria epidemiology. American society of tropical medicine and hygiene 2007, 76:450-460.
17. Watson M: The prevention of malaria in the Federated Malay States, a record of 20 years progress. New York: E.P. Dutton and company; 1921.
18. Jomon KV, Valamparampil TT: Medically important mosquitoes in the rubber plantation belt of central Kerala, India. Southeast Asian J Trop Med Public Health 2014, 45:796.
19. Sumodan PK: Potential of rubber plantations as breeding source for Aedes albopictus in Kerala, India. Dengue Bull 2003, 27:197-198.
20. Sumodan PK: Species diversity of mosquito breeding in rubber plantations of Kerala, India. J Am Mosq Control Assoc 2012, 28:114-115.
21. Rosenberg R, Andre RG, Somchit L: Highly efficient dry season transmission of malaria in Thailand. Trans R Soc Trop Med Hyg 1990, 84:22-28.
22. Obsomer V, Defourny P, Coosemans M: The Anopheles dirus complex: spatial distribution and environmental drivers. Malaria Journal 2007, 6.
23. Gratz NG: Critical review of the vector status of Aedes albopictus. Med Vet Entomol 2004, 18:215-227.
24. Paupy C, Delatte H, Bagny L, Corbel V, Fontenille D: Aedes albopictus, an arbovirus vector: from the darkness to the light. Microb Infect 2009, 11:1177-1185.
25. Kaewwaen W, Bhumiratana A: Landscape ecology and epidemiology of malaria associated with rubber plantations in Thailand: integrated approaches to malaria ecotoping. Interdiscip Perspect Infect Dis 2015, Article ID 909106:17.
26. Bhumiratana A, Sorosjinda-Nunthawarasilp P, Kaewwaen W, Maneekan P, Pimnon S: Malaria-associated rubber plantations in Thailand. Travel Med Infect Dis 2013, 11:37-50.
27. Pattanasin S, Satitvipawee P, Wongklang W, Viwatwongkasem C, Bhumiratana A, Soontornpipit P, Jareinpituk S: Risk factors for malaria infection among rubber tappers living in a malaria control program area in southern Thailand. Southeast Asian J Trop Med Public Health 2012, 43:1313-1325.
28. Bigoga JD, Nanfack FM, Awono-Ambene PH, Patchoké S, Atangana J, Otia VS, Fondjo E, Moyou RS, Leke RGF: Seasonal prevalence of malaria vectors and entomological inoculation rates in the rubber cultivated area of Niete, South region of Cameroon. Parasit Vectors 2012, 5:197.
29. Satitvipawee P, Wongkhang W, Pattanasin S, Hoithong P, Bhumiratana A: Predictors of malaria-association with rubber plantations in Thailand. BMC Public Health 2012, 12:1115
30. Hiscox A, Kaye A, Vongphayloth K, Banks I, Khammanithong M, Sananikhom P, Kaul S, Hill N, Lindsay S, Brey P: Risk factors for the presence of Stegomyia aegypti and Stegomyia albopicta in domestic water-holding containers in areas impacted by the Nam Theun 2 hydroelectric project, Laos. Am J Trop Med Hyg 2013, 88:1070-1078.
31. Kay B, Nam VS: New strategy against Aedes aegypti in Vietnam. Lancet 2005, 365:613-617.
32. Jennings CD, Phommasack B, Sourignadeth B, Kay BH: Aedes aegypti control in the Lao People’s Democratic Republic, with reference to copepods. Am J Trop Med Hyg 1995, 53:324-330.
33. Rueda LM, Vongphayloth K, Pecor JE, Sutherland IW, Hii J, Debboun M, Brey PT: Mosquito fauna of Lao People’s Democratic Republic, with special emphasis on the adult and larval surveillance at Nakai district, Khammuane province. US Army Med Dep J 2015, July-September: 25-32.
34. Chen-Hussey V, Carneiro I, Keomanila H, Gray R, Bannavong S, Phanalasy S, Lindsay SW: Can topical insect repellents reduce malaria? A cluster-randomised controlled trial of the insect repellent n,n-diethyl-m-toluamide (deet) in Lao PDR. PLoS One 2013, 8:e70664.
35. Hiscox A, Khammanithong P, Kaul S, Sananikhom P, Luthi R, Hill N, Brey PT, Lindsay SW: Risk factors for mosquito house entry in the Lao PDR. PLoS ONE 2013, 8:e62769.
36. Vythilingam I, Sidavong B, Chan ST, Phonemixay T, Vanisaveth V, Sisoulad P, Phetsouvanh R, Hakim SL, Phompida S: Epidemiology of malaria in Attapeu Province, Lao PDR in relation to entomological parameters. Trans R Soc Trop Med Hyg 2005, 99:833-839.
37. Phetsouvanh R, Vythilingam I, Sivadong B, Hakim S, Chan ST, Phompida S: Endemic malaria in four villages in Attapeu Province, Lao PDR. Southeast Asian J Trop Med Public Health 2004, 35:547-551.
38. Vythilingam I, Phetsouvanh R, Keokenchanh K, Yengmala V, Vanisaveth V, Phompida S, Hakim SL: The prevalence of Anopheles (Diptera: Culicidae) mosquitoes in Sekong Province, Lao PDR in relation to malaria transmission. Trop Med Int Health 2003, 8:525-535.
39. Tsuda Y, Kobayashi J, Nambanya S, Miyagi I, Toma T, Phompida S, Manivang K: An ecological survey of dengue vector mosquitos in central Lao PDR. Southeast Asian J Trop Med Public Health 2002, 33:63-67.
40. Toma T, Miyagi I, Okazawa T, Kobayashi J, Saita S, Tuzuki A, Keomanila H, Nambanya S, Phompida S, Uza M, Takakura M: Entomological surveys of malaria in Khammouane Province, Lao PDR, in 1999 and 2000. Southeast Asian J Trop Med Public Health 2002, 33:532-546.
41. Vythilingam I, Sidavong B, Chan ST, Phonemixay T, Phetsouvanh R, Phompida S: Heavy natural oocyst infections in Anopheles dirus (Diptera: Culicidae) from Attapeu province, Lao PDR. Int J Trop Insect Sci 2001, 25:59-61.
42. Vythilingam I, Keokenchan K, Phommakot S, Nambanya S, Inthakone S: Preliminary studies of Anopheles mosquitos in eight provinces in Lao PDR. Southeast Asian J Trop Med Public Health 2001, 32:83-87.
43. Kobayashi J, Somboon P, Keomanila H, Inthavongsa S, Nambanya S, Inthakone S, Sato Y, Miyagi I: Malaria prevalence and a brief entomological survey in a village surrounded by rice fields in Khammouan province, Lao PDR. Trop Med Int Health 2000, 5:17-21.
44. Kobayashi J, Vannachone B, Sato Y, Sinjo M, Nambanya S, Manivang K, Inthakone S: Current status of malaria infection in a Southeastern province of Lao PDR. Southeast Asian J Trop Med Public Health 1998, 29:236-241.
45. Kobayashi J, Nambanya S, Miyagi I, Vanachone B, Manivong K, Koubouchan T, Amano H, Nozaki H, Inthakone S, Sato Y: Collection of anopheline mosquitos in three villages endemic for malaria in Khammouane, Lao PDR. Southeast Asian J Trop Med Public Health 1997, 28:20-21.
46. Pholsena K: The malaria situation and antimalaria program in Laos. Southeast Asian J Trop Med Public Health 1992, 23:39-42.
47. Mayxay M, Castonguay-Vanier J, Chansamouth V, Dubot-Pérès A, Paris DH, Phetsouvanh R, Tangkhabuanbutra J, Douangdala P, Inthalath S, Souvannasing P, et al: Causes of non-malarial fever in Laos: a prospective study. Lancet Glob Health 2013, 1:e46-e54.
48. Phetsouvanh R, Sonthayanon P, Pukrittayakamee S, Paris DH, Newton PN, Feil EJ, Day NPJ: The diversity and geographical structure of Orientia tsutsugamushi strains from scrub typhus patients in Laos. PLoS Negl Trop Dis 2015, 9:e0004024.
49. Stekolnikov AA: A new genus and two new species of chigger mites (Acari: Trombiculidae) from the Laotian rock-rat Laonastes aenigmamus Jenkins, Kilpatrick, Robinson & Timmins (Rodentia: Diatomyidae). Syst Parasitol 2014, 87:21-31.
50. Phongmany S, Rolain J-M, Phetsouvanh R, Blacksell SD, Soukkhaseum V, Rasachack B, Phiasakha K, Soukkhaseum S, Frichithavong K, Chu V, et al: Rickettsial infections and fever, Vientiane, Laos. Emerg Infect Dis 2006, 12:256-262.
51. Léger N, Depaquit J, Gay F: Chinius eunicegalatiae n. sp. (Diptera; Psychodidae), a cavernicolous sandfly from Laos. Ann Trop Med Parasitol 2010, 104:595-600.
52. Kernif T, Socolovschi C, Wells K, Lakim MB, Inthalad S, Slesak G, Boudebouch N, Beaucournu J-C, Newton PN, Raoult D, Parola P: Bartonella and Rickettsia in arthropods from the Lao PDR and from Borneo, Malaysia. Comp Immunol Microbiol Infect Dis 2012, 35:51-57.
53. Trpis M: Consequences of vector behavior in epidemiology of Onchocerciasis on the firestone rubber plantation in Liberia. Am J Trop Med Hyg 2006, 74:833-840.
54. Taylor H, Pacque M, Munoz B, Greene B: Impact of mass treatment of onchocerciasis with ivermectin on the transmission of infection. Science 1990, 250:116-118.
55. World Health Organization: World malaria report 2015. In World Malaria Report 2015. Geneva: WHO; 2015.
56. WHO Factsheet Vector-borne diseases, Factsheet # 387 [http://www.who.int/kobe_centre/mediacentre/vbdfactsheet.pdf]








