Pertussis in Lao PDR: Seroprevalence and disease
Nai ban (village head) in Champasack reading project information sheet during COVID-19 study. He is sitting in the village office, under a COVID-19 information poster.
Project coordinators: Daria Kleine (LIH), Phonethipsavanh Nouanthong (IPL)
Partners: Luxembourg Institute of Health, Children’s Hospital, Vientiane, Lao Red Cross, National Centre for Laboratory and Epidemiology, Vientiane
Background
Whooping cough or pertussis, a highly infectious disease that mainly occurs in children, is caused by the gram-negative bacteria Bordetella pertussis. Symptoms such as fever, runny nose and cough, occur within seven to ten days after exposure and develop into a paroxysmal cough followed by whooping. Symptoms are often uncharacteristic, including apnoea, cyanosis and lymphocytosis and may not be recognized early on. Complications include pneumonia, otitis media, encephalitis or convulsions. In children, pertussis is more severe than in adults. Adults who were never vaccinated or have lost their immunity can be a reservoir for B. pertussis and potential sources of infection for children. If the mother has sufficient antibodies against pertussis toxin (anti-PT), transplacentally acquired antibodies may protect new-borns during the first months of their lives.
Lao PDR has the highest mortality rate in under 5-year olds within the Association of Southeast Asian Nations, and 63.9 deaths per 1000 live births. DTP-vaccine was first introduced in two provinces, Vientiane and Savannakhet, in 1979. Nationwide DTP-vaccination was implemented in 1989, but coverage reached only 60% by 2008, 89% in 2015 and 82% in 2016. In 1990, pertussis caused 2.7% of premature deaths in Lao PDR, but decreased ranking of the causes of premature deaths from rank 22 to rank 33 by 2010. In 2009, the country switched from the DTP vaccine to the pentavalent vaccine (containing in addition hepatitis B and haemophilus influenzae components) given at 6, 10 and 14 weeks of age. Both vaccines contain a whole-cell pertussis emulsion (wP).
In a previous study, we showed that the low seroprevalence of other components of the pentavalent vaccine was not only due to low vaccination coverage but also to a low response to the vaccine.
Outbreaks of pertussis were reported in 11 of 17 provinces throughout Lao PDR between 2011 and 2017. The WHO describes disease surveillance for B. pertussis in Lao PDR as inadequate.
In this study, we aim to investigate the current epidemiological situation in Lao PDR in order to estimate disease susceptibility, age-dependent incidence and to develop strategies to mitigate pertussis outbreaks and reduce child mortality.
Methods
Study participants
This study included 7 cohorts (n=3547). Informed consent was obtained from all participants or their parents/guardians. In the cohort descriptions, vaccination coverage refers to three vaccine doses during the first year of life. Outbreak data are obtained from Bouaphan Khamphaphongphone, NCLE. Data about vaccine coverages was received from Dr. Anonh Xeuatvongsa, NIP-MHCH, Lao PDR and the Gavi Vaccine Alliance.
Children with documented vaccination.
Children aged 3 months to 5 years with 3 documented doses of pentavalent vaccine were recruited from Vientiane Capital, Bolikhamxay and Khammouane provinces in 2013/14 as described previously (n=958, ethics approval number NECHR 860/2013. Antibodies against tetanus were used as a marker for vaccination. Antibodies against diphtheria and hepatitis B surface antigen were used for comparison of immunogenicity.
Pre-school children.
117 pre-school children aged 1 to 5 years of age were recruited in 2013 from Xamtai and Kuan districts of Huaphan Province as described previously (ethics approval number NECHR 732/2013). Immunization status was known from 101 participants, including 66 fully immunized children. Vaccination coverage of the children with unknown immunization status was estimated at 44% to 95%.
Schoolchildren.
Schoolchildren aged 6 to 19 years (n=671) were recruited from Luangprabang, Savannakhet and Bolikhamxay provinces.
The recruitment was school-based as part of a study on measles/rubella vaccine coverage in 2011/12 (ethics approval number NEHCR 001/2011). Their individual immunization status is unknown, but vaccination coverage was estimated to be up to 54% in Luangprabang, 74% in Savannakhet and 56% in Bolikhamxay.
Blood donors.
Adult blood donors 19 to 65 years of age (n=517) were recruited between 2013 and 2015 from Xayaboury, Huaphan, Luangnamtha, Khammuane, Attapeu, Luangprabang provinces and Vientiane Capital (ethics approval number NEHCR 059/2014). Their immunization status is unknown. Vaccination coverage was estimated as 54% for those between 20 and 23 years of age. Those older than 38 years in Vientiane and older than 25 years in other provinces were born before the DTP-introduction.
Healthcare workers (HCW).
Adult HCW (n=469) were recruited from 3 central, 2 provincial and 8 district hospitals within Vientiane Capital in 2013 as described previously (ethics approval number NEHCR 038/2013). Their immunization status is unknown. Vaccination coverage was estimated to be up to 54% for those under 35 years, while those older than 35 years were born before the DTP-introduction.
Pregnant women and paired cord blood. A serum of 170 pregnant women aged 15 to 42 years and paired cord blood samples was obtained from Savannakhet province in 2017 as part of a study on maternal-neonatal tetanus. Women were recruited whilst attending district hospitals for delivery (ethics approval number NEHCR 046/2017). Their immunization status is unknown. There was an estimated provincial vaccination coverage of up to 74% for those younger than 38 years of age, while those older were born before the vaccine introduction in Savannakhet.
Symptomatic children.
In 2014/2015, throat swabs and nasopharyngeal aspirates were collected from 475 children aged 0-15 years, presenting at the Children Hospital in Vientiane with fever (n=411), cough (n=429) and/or rhinorrhea/nasal congestion (n=443). All had unknown immunization status (027/NIOPH/ NECHR/2015).
Serology
All serum samples (n=3072) were analysed by commercial ELISA (EUROIMMUN, Lübeck, Germany) for anti-PT IgG. According to the manufacturer’s instructions and previous studies, titres are indicative of vaccination and infection histories. Thus; <5 IU/mL corresponded to seronegativity; 5 to 40 IU/mL, infection or vaccination more than 12 months before; 40 to 100 IU/mL, infection or vaccination within the past 12 months; ≥ 100 IU/mL, acute infection or recent vaccination. Although a high antibody level of anti-PT IgG is associated with protection against B. pertussis, a protective titre has not been defined. Antibodies against tetanus toxin (anti-TT Ig) were measured by commercial ELISA (EUROIMMUN, Lübeck, Germany).
PCR
For symptomatic children, nasal swabs and nasopharyngeal aspirates were analysed for the presence of B. pertussis by a multiplex conventional PCR. DNA was extracted from pooled paired samples using Trizol LS (Life Technologies, Thailand) and Pure Link Viral RNA/DNA Mini Kits (Life Technologies, Belgium). Statistics
Data were entered into Excel and analysed by SPSS. Proportions of different groups were compared by Chisquare tests. Logistic regression was used to estimate crude and adjusted odd ratios (OR) with 95% confidence interval (CI). P-values <0.05 were considered significant.
Results
Children with documented vaccination (aged 3 months-5 years)
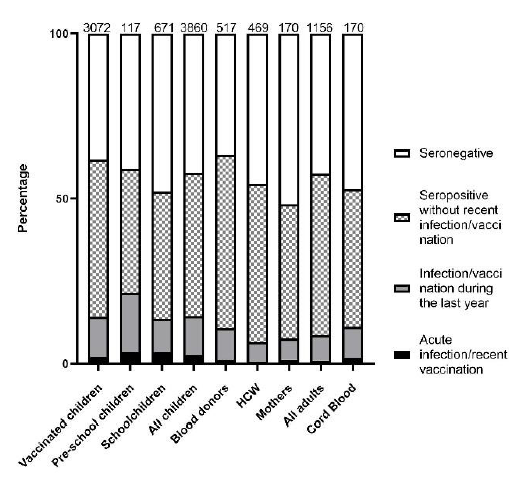
Despite three documented doses of pentavalent vaccine, overall seronegativity was very high (38.2%; Figure 7). Even when using the TT-status as a marker for vaccination, 217/787 (27.6%) TT-positive children were seronegative for anti-PT IgG. Serology indicating vaccination (or infection) within the last 12 months was low (14.3%).
In children vaccinated within the last 12 months, there were significant differences in immunity levels between provinces and vaccine components (Figure 2). While children from Khammouane had lower immunity against diphtheria (50.0%) and hepatitis B (46.2%) than children from Vientiane (64.9%, P=0.027; 52.6%, P>0.05, respectively), their anti-PT IgG seroprevalence was significantly higher (74.2% and 57.8%, respectively, P=0.018). This is suggestive of pertussis infections in Khammouane e.g. during a reported outbreak there at the time of sample collection, rather than better vaccine immunogenicity.
Overall, seronegativity was higher in those with documented vaccination > 20 months ago (42.5%), compared with those documented vaccinated within the last 12 months (32.1%; P=0.009; Figure 2), suggestive of antibody waning. The prevalence of titres indicating vaccination/infection within the last 12 months was not significantly different according to time since vaccination (13.4% and 16.7%; P=0.77; Figure 8), further suggesting pertussis infections.
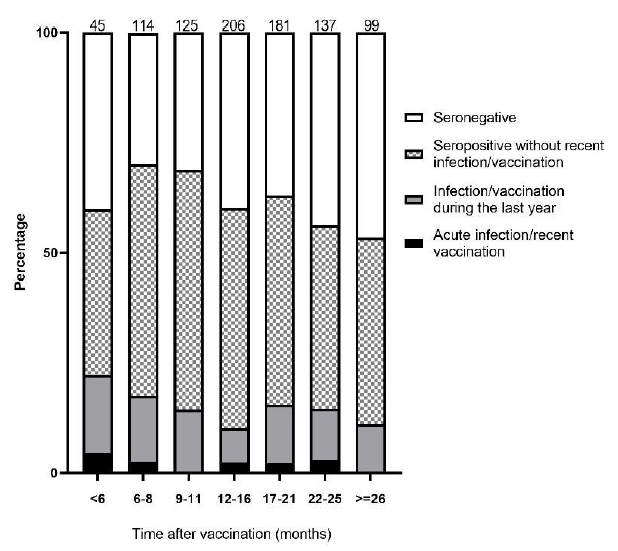
Figure 8. Pertussis
Pre-school children in Huaphan province (1 to 5 years old)
The highest rates of serology indicative of recent infection/vaccination (3.4%) and <12 months of infection/ vaccination (18.0%) were found in this cohort. Also, 37.6% had antibody titres suggesting infection/vaccination >12 months before and 41% were seronegative (Figure 1). In Xamtai district, closer to the nearest health facility, there was significantly higher seropositivity (38/53; 71.1%) compared to Kuan district (30/63; 47.6%, P=0.009). A longer distance to the health facility (P=0.007) and living in a household with <7 members (P=0.037), had a higher rate of titres showing infection/vaccination <12 months ago. Schoolchildren
Schoolchildren (age 6-19 years)
In this cohort, titres above 40 IU/mL were interpreted as infections during the last year, since the vaccination was more than 5.5 years previously. Approximately half of the schoolchildren were seropositive (52.16%), including 10.28% with titres indicating infections <12 months and 3.34% indicating recent infections (Figure 1). A reported pertussis outbreak in Savannakhet in 2011/12 is compatible with high seropositivity and recent infections. Seropositivity in Savannakhet (65.2%), as well as serology showing recent infections and infections <12 months (24.8%), were significantly higher than in Bolikhamxay (44.2% and 9.4%; p<0.001) and Luangprabang (48.2% and 7.9%; p<0.001). In Bolikhamxay, the seropositivity rate was significantly higher in 13- to 19-year olds (53%) than in 6- to 12-year olds (37.6%; p=0.018), indicative of ongoing unreported outbreaks in these age groups. Thus, pertussis affects schoolchildren all through their adolescent life in all three provinces.
Adult blood donors
For the adult cohorts, a seropositive result is more likely to be due to past infection, since the last vaccination was more than 14 years previously. Of the blood donors who were born before vaccine introduction in 1979 (Vientiane)/1989 (nationwide), 61.64% (188/305) were seropositive, suggesting a high incidence of pertussis during their childhood and more recently (11.5%). A reported outbreak in Khammouane in 2012/13 is compatible with significantly higher seropositivity in this province (85/115; 73.9%) than in Attapeu (69/118; 58.5%, p=0.037) or Vientiane (70/129; 54.3%, p=0.026).
Healthcare workers
The seroprevalence in HCW was similar to the other adult cohorts (Figure 1). They had a relatively low prevalence of titres indicating recent (0.6%) and <12 months (6.0%) infections. Notably, 45.4% were seronegative and susceptible to disease.
Mother and cord blood
There was a highly significant correlation between the mothers’ titre and the paired cord blood (R value = 0.8148, P=<0.001; Figure 3). 3/170 women (1.2%) had antibody titres indicative of acute infections. Half of the mothers were seronegative (51.7%; Figure 1), also leaving their babies unprotected. A reported outbreak in Savannakhet 5 years before sample collection suggests that circulation in this province is high, increasing the risk of infection for the new-borns.
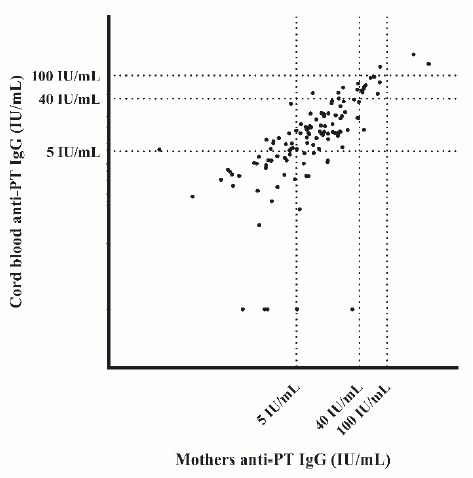
Figure 9. Pertussis
Symptomatic children
B. pertussis was detected in 1.05% (5/475) of children who presented with respiratory symptoms. The B. pertussis positive children were between 3 and 13 years old (mean=7). Two cases were detected in March 2015 and three other cases occurred in June 2015.
Discussion
This study is the first to address the epidemiology of pertussis in Lao PDR, the country with the highest disease specific mortality in South-East Asia.
Despite three documented doses of the pentavalent vaccine, only two thirds of vaccinees aged 3 months to 5 years were seropositive. This is similar to low immunogenicity against other components of the vaccine in this cohort. Due to waning antibodies, the percentage of children protected by the vaccine will further decrease. In the other child cohorts, including the pre-schoolers, vaccination coverage was low. Nevertheless, these cohorts had a higher incidence of titres ≥40 and ≥100 IU/mL. This serology paired with many seronegative is suggestive of poor vaccine response/coverage followed by wildtype infection. Low vaccine response/coverage was particularly a problem for children living further away from the health care facility. Vaccination of pre-schoolers living in more remote areas is conducted by outreach teams, transporting the vaccine from the nearest health care facility to the villages, explaining why vaccination may be less robust and the disease burden higher.
High seronegativity in schoolchildren aged 6 to 19 years indicates incomplete vaccine response, coverage and waning of immunity. Since this cohort was vaccinated at least 5 to 6 years earlier, the high prevalence of titres ≥40 IU/mL indicates high pertussis incidence. In Savannakhet, high titres in schoolchildren and also in elder children and adults are compatible with the outbreak reported before or during the sample collection.
Adult blood donors had a lower rate of titres indicative of acute infections (1.16%) and infections <12 months (9.7%) than the pre-school children and schoolchildren, but it was higher than in Thailand (6.3%) and in Europe (1%-6%) during the 1990s. There was a high percentage of blood donors with titres indicating infection >12 months earlier (52.42%) and a lower proportion of seronegative (36.8%). Seropositivity in this age group is comparable to other countries such as Mexico with 50% and 47.6% seropositive, respectively.
We find that a significant proportion of HCW is susceptible to pertussis and at potential risk of infection from their patients. This is in line with our previous reporting of a high susceptibility of HCW in Lao PDR to other vaccine preventable infections. It is comparable to other studies addressing the susceptibility of HCW to pertussis.
Finally, we observed a significant correlation in antibody levels between pregnant women and cord blood, confirming the trans-placental transfer of protective antibodies. Approximately half of women and cord blood were seronegative and therefore susceptible to infection. For this reason, some countries recommend an antenatal vaccination with the pertussis-containing vaccine. So far, there is no such recommendation in Lao PDR, but there are no previous data about pertussis in newborns and infants. While aP vaccines could interfere with childhood vaccination response, wP vaccines may have higher immunogenicity and the benefit of this is still under investigation.
In a study in Thailand, 6.3% of over 11-year old children were infected during the 12 months. Using their cut-off of 40IU/ml, we estimate infections in 10.3% (186/1799) of over 7 year-olds in Lao PDR. This corresponds to an estimated incidence of 10339/100,000 in this population, similar to an estimated 9395/100,000 in Guangdong province in China. In our study, the detection of B. pertussis in symptomatic children from Vientiane (1.05%) confirmed the active circulation of B. pertussis at least in this age group.
Despite serological evidence of high pertussis incidence, less than 50 annual cases have been reported from 2016 to 2018. While 1726 pertussis cases were notified from eleven provinces throughout Lao PDR since 2011, there was none reported from Vientiane capital (NCLE). As in other countries, there seems to be a considerable underreporting of pertussis cases in Lao PDR.
Conclusion
Serology suggests that the incidence of pertussis is high in under-fives and infection continues in teenagers and even in adults. This seems to be due to low vaccine response especially after outreach vaccination and to rapid antibody waning. In adults born before the introduction of pertussis containing vaccines the seroprevalence can be as high as 75% but less than 50% in HCW. Thus, systematic vaccination of HCW, especially for those in neonatal care, should be considered. More importantly, booster for pregnant women during antenatal care and for children before the age of 5 years is recommended. There is also a need to strengthen the reporting of this highly prevalent notifiable disease. Pertussis diagnostic should be introduced at least in one central facility. These data and recommendations have been formulated as a policy brief and reported to the Lao Ministry of Health and published as a manuscript.
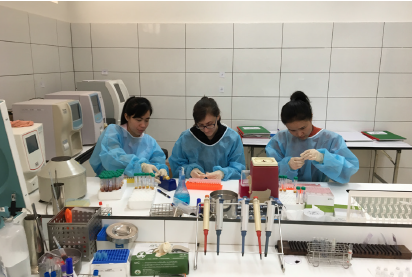
Vilaysone Khounvisith (IPL), Lisa Hefele (LIH) and
Souphaphone Vannachone (LTPHI) processing samples for
HBV vaccine impact study, Provincial Hospital, Bolikhamxay







