Positive impact of HBV vaccination in Lao PDR
Vilaysone Khonvisith and a teacher during recruitment of adolescents from schools in Bolhikhamxay for the HBV impact study
Project coordinators: Lisa Hefele (LIH), Souphaphone Vannachone (LTPHI)
Partners: Luxembourg Institute of Health, Lao Tropical Public Health Institute
Background
The introduction of HBV vaccines into the national immunization schedule in Lao PDR started in 2001/2, with three doses at 6, 10 and 14 weeks, followed by the introduction of the HBV birth dose in 2003/4, although dates vary according to sources. Currently, the three HBV vaccination doses are part of a pentavalent vaccine, a combination with diphtheria, tetanus, pertussis and Haemophilus influenzae b (DTPw-HepB-Hib). The majority of HBV infections occur perinatally and during early childhood when the risk of chronic infection is highest. Therefore, high coverage with the birth dose (monovalent) is crucial to prevent chronic infection. There is little information about the uptake of the birth dose during the years early after its introduction but even in 2017, the nationwide coverage was only 55%. The percentage of children with 3 doses of the DTPHepB vaccine (DTPw-HepB-Hib since 2009) increased gradually from 57% in 2006 to 89% in 2014 and 85% in 2017.
In addition to coverage, vaccine response was as low as 37.9% in a study in 2013/14. However, recent improvements of the immunization program and vaccine management resulted in a dramatic increase in vaccine response and typical protection levels against infection and chronic disease in small children.
In 2011, we reported that 17% of school students (age 5-19) from three different provinces had a past infection and 3.6% were chronically infected. Less than 20% had antibodies against the hepatitis B surface antigen (anti- HBs) in absence of antibodies against the hepatitis B core antigen (anti-HBc), indicating vaccination.
In the current study, 17 years after the introduction of HBV vaccination, we assessed the long-term benefit of HBV vaccination for adolescents. Adolescents aged 11 to 18 years in 2018 were born at the time of and after the introduction of the HBV vaccination in Lao PDR. We aimed to investigate the impact of vaccination on protection rates and persistence of infections before they enter into the next phase in their lives with new risks of HBV exposure.
Methods
The study was approved by the Lao National Ethics Committee (Reference number 022/NECHR) and the Institutional Review Board of the Institut Pasteur (Reference number 9).
Participants
Between March and June 2018, 4 and 5 schools were selected in Vientiane Capital and in two districts of Bolikhamxay province, respectively, based on a number of students and location of a previous base-line study. Students between the age of 11 and 18 years were randomly selected in order to have the same age and gender ratios in both provinces. In total, 388 students were enrolled in Vientiane Capital (urban), 197 students in Paksan, the Capital of Bolikhamxay (urban) and 194 students in Pakkading district (semi-urban). All parents/ guardians signed the informed consent form and participants could withdraw their participation at any time. Age, gender, vaccination history, history of liver disease in the family and other potential risk factors were collected digitally on a tablet using Kobotoolbox. Since some of the participants were uncertain about their date of birth, the birth year was calculated by subtracting the age that they stated in the questionnaire from the year of sample collection. As a control, birth dates were matched with calculated birth years and the discrepancy was >1 year only for less than 5% of the participants. Data from the current study were compared to data collected in 2011. In this study, 560 schoolchildren aged 5-19 years participating in a 2011 national immunization campaign against measles and rubella were recruited. The students were not randomly selected. From this cohort, 386 students from Bolikhamxay between 11 and 18 years were selected for the comparison to the 2018 data. In 2011, no data was available from Vientiane Capital in this age group.
Laboratory analyses
After informed consent, 5 ml blood was collected from each participant by a health care worker. Serum was separated by centrifugation on the day of the sample collection and stored at -20°C for a maximum of two months, before being transferred to long-term storage at -80°C. All samples were tested on the day of the sample collection with a rapid test for the hepatitis B surface antigen (HBsAg; ONE STEP HBsAg TEST, SD BIOLINE), which is a marker for acute or chronic infection. Results and information regarding HBV infection were handed out in closed envelopes to the students. In case students were found to be positive for HBsAg, they were recommended to seek medical advice and to confirm the rapid test result. Commercial ELISA kits were used to determine anti-HBs (quantitative; Diasorin) and anti- HBc (qualitative; Diasorin) antibodies. The presence of anti-HBs antibodies in absence of anti-HBc antibodies indicates protection through vaccination, while the presence of anti-HBc antibodies indicates infection with HBV. Anti-HBc positive and anti-HBs negative sera were tested for HBsAg (qualitative; Diasorin). An anti-HBs titer ≥10 IU/L was considered protective.
The serum samples collected during the study in 2011 were tested with the same commercial ELISA kits (Diasorin, Italy).
Statistical analyses
Data analyses were conducted using R software with the following packages: “stats”, “MASS”, “epitools”, “fmsb”, “lmtest”, “rcompanion”, “pROC”, “tidyverse” and “car”. Data from 2018 was compared between Vientiane Capital and Bolikhamxay province for all age groups specified. Data from Bolikhamxay in 2018 was compared to data collected in 2011 from the same age group.
In order to identify variables potentially associated with the antibody status, bivariate analyses were performed. Chi-square test and Fisher’s exact test were applied to assess which factors are associated with seroprotection. Odds Ratio (OR), 95% confidence interval (CI) and p-values were calculated. Only variables with p-values <0.2 were included in the models. A correlation value >0.5 or a variance inflation factor >5 was considered as correlation and the decision to exclude the variable was made on a case-by-case basis: the variable which was deemed to be less important and/or with the lower impact was removed.
Binary regressions were performed using a stepwise method for removing variables that were not associated with the response variable one by one, taking both the p-value of the variable and the Akaike Information Criterion (AIC) of the model into consideration. The significance of the final model in comparison with the null model was tested using a likelihood ratio test (R function “anova” with argument test set to “Chisq”). In addition, the individual effect of the variables in the model was tested by Wald tests (R function “Anova” with argument test. statistics set to “Wald”).
Results
Participants in 2018
The majority of the students lived with their parents (85.9%). 46.9% of the students in Vientiane Capital and 50.6% in Bolikhamxay were male. In Vientiane Capital, nearly half of the students (47.7%) were born in a Central hospital in the Capital and only 7.5% were born at home. Nearly all students were of Tai-Kadai ethnicity (98.5%). In Bolikhamxay province, only 2.8% of the students were born in a Central hospital, 16.1% were born in a Provincial hospital and more than one third (38.1%) of the participants was born at home. In the province, 7.2% of the students were of Hmong-Mien, Mon-Khmer or another non-Tai-Kadai ethnicity. A large proportion of the students did not know their place of birth (26.6% in Bolikhamxay, 37.9% in Vientiane Capital). None of the participants stated to have used intravenous drugs and only two – in Vientiane Capital – stated to have a tattoo. 2.6% of all students had received a blood transfusion and 6.3% stated that they were aware of chronic liver disease in their family. The questions regarding sexual relationships were only asked students >13 years. In both provinces, 13.5%-14% stated to have had a sexual relationship starting at the age of 14 years. About half of those with previous relationships stated to have had more than one partner in the past 6 months. Documentation of previous vaccinations, such as the yellow immunization cards, were not available for all but three students.
Serological profiles
Overall serology profiles
In 2018, the overall anti-HBc seroprevalence was 6.4% and 12.6% in Vientiane Capital and Bolikhamxay province, respectively (p<0.01, Table 10). In Bolikhamxay, this is a significant decrease compared to the same age group in 2011 (19.2%, p<0.05) – all born before vaccine introduction. In addition, the HBsAg prevalence in 2018 was significantly lower in Vientiane Capital than in Bolikhamxay (1.6% vs. 4.4%, p<0.05, Table 10). However, there was no statistical difference between Bolikhamxay in 2018 and 2011, when 3.4% of the students tested positive for HBsAg. The serological profile typical for vaccination (anti-HBs+/anti-HBc-) was only somewhat higher in Vientiane Capital than in Bolikhamxay in 2018 (19.3% vs 15.4%), and the difference was not significant (Table 10). The proportion of students negative for both anti-HBc and anti-HBs was similar in Vientiane and Bolikhamxay and increased significantly in Bolikhamxay from 61.4% in 2011 to 72.1% in 2018 (p<0.01).
Table 10. HBV profiles of students aged 11-18 years according to study year and study site
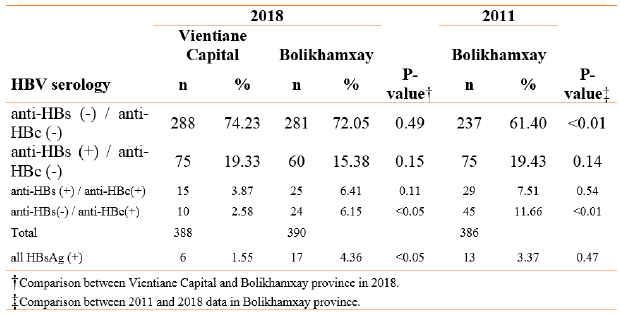
Serological profiles by birth cohort
HBV vaccination was gradually introduced into the national immunization program from 2001 onwards. Figure 5A and 5B show the serological profiles by year of birth in Vientiane capital and Bolikhamxay province in 2018. In Vientiane, there is a visible increase in the serological profile for vaccination already in 2003, while in Bolikhamxay it took a year longer (Figure 5). If we compare serological markers for vaccination (anti- HBs+/anti-HBc-) before and after these dates, we find an increase of 12.2% to 25% (p<0.01) in Vientiane and from 3.4% to 28.5% (p<0.00001) in Bolikhamxay. The decline of anti-HBc(+) students was also significant at both recruitment sites between these years (9.3% vs. 4.2%, p<0.05 in Vientiane Capital and 18.1% vs. 6.5%, p<0.001 in Bolikhamxay). In Bolikhamxay province, but not in Vientiane, also the decrease of HBsAg(+) students was significant (6.4% vs. 2.1%, p<0.05). There was no statistical difference between the proportion of students with the serological vaccination profile born after the visible impact of the vaccine in Vientiane Capital (2003- 2007) and Bolikhamxay Province (2004-2007) (28.5% in Bolikhamxay vs. 25% in Vientiane Capital, p=0.43).
Even when only those students born before or in 2001, the year of the introduction of the vaccine, were compared to those students born after this date, the prevalence of students with serological evidence of vaccination increased from 13.2% to 21.9% (p<0.05) in Vientiane and from 3.0% to 19.7% (p<0.001) in Bolikhamxay. At the same time, serological evidence of previous infection declined from 11.4% to 4.4% in Vientiane (p<0.05) and 22.0% to 9.3% (p<0.01) in Bolikhamxay. The prevalence of HBsAg did not decrease significantly in Vientiane or Bolikhamxay.
When students of the same age (11-14 years old) from Bolikhamxay in 2011 (Figure 5C) were compared to 2018, the proportion of students with a serological vaccination profile was considerably higher in 2018, after the introduction of the vaccination (28.5% vs. 17.6%, p<0.05). The proportion of students that were HBc(+) was also dramatically lower in 2018 compared to 2011 (6.5 vs. 20.1%, p<0.001). However, the prevalence of HBsAg(+) students was not significantly different in 2018 in this age group (6.5% in 2018 vs. 6.2% in 2011, p=0.56).
The prevalence of the vaccination profile was around 25-30% in Bolikhamxay province in the 2011 data in participants born in 2002-2004 as compared to 3.5- 22.6% in participants born in the same years in the 2018 study (Figure 5). Since participants born in 2002-2004 were 14-16 years old by 2018, this discrepancy is likely due to antibody waning over time.
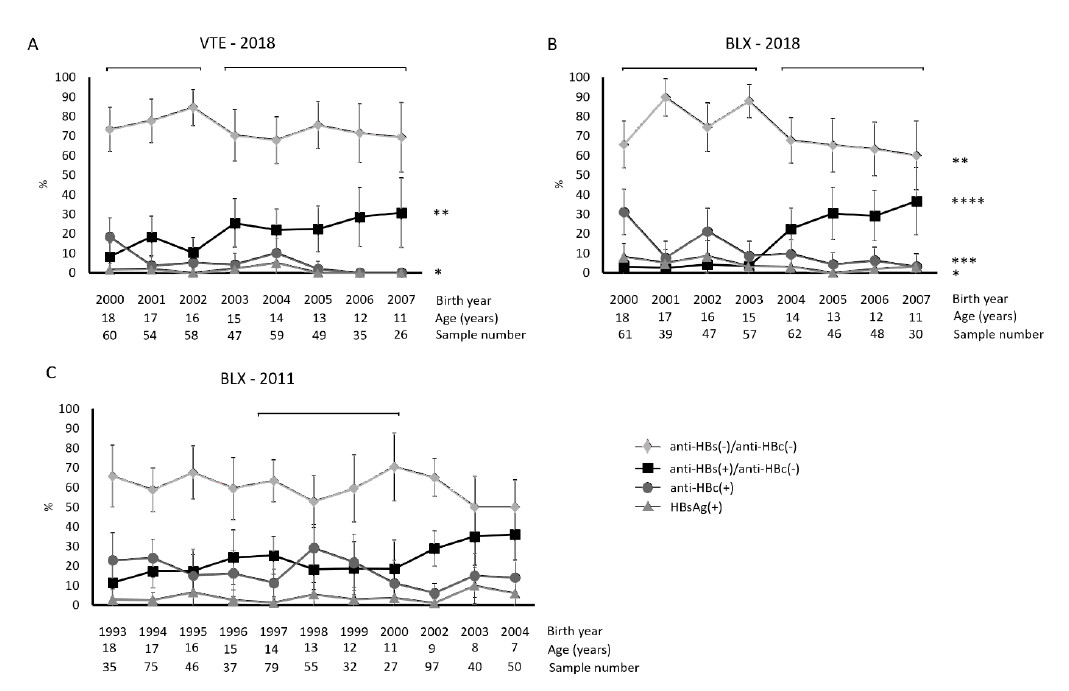
Figure 5. Hepatitis B serological profiles in A Vientiane Capital in 2018, B Bolikhamxay province in 2018 and C Bolikhamxay province in 2011. Data points are presented with 95% CIs. * = p <0.05; ** = p <0.01, *** = p <0.001, **** = p <0.0001. In panel A, * relates to the line corresponding to the prevalence of anti-HBc(+), in panel B, * relates to the line corresponding to the prevalence of HBsAg. In panel C, data from 2001 was omitted due to low sample numbers. The brackets above the serological profiles indicate the birth year cohorts that were compared with each other. Abbreviations: VTE, Vientiane; BLX, Bolikhamxay.
Bivariate analyses of 2018 data
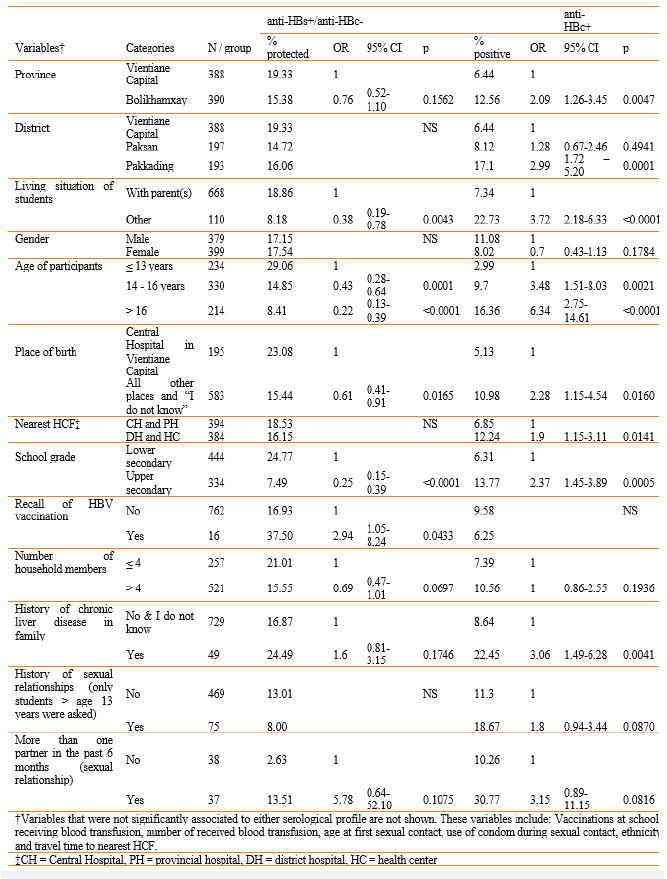
Bivariate analyses were performed on the 2018 data to investigate factors associated with the typical vaccination serology as well as HBV infection. In 2018, age >13 years, not living with parents, not born in a central hospital and being in an upper school class were negatively associated with the vaccination serology while recall of HBV vaccination was positively associated (p<0.05). All variables associated with the vaccination profile with a p<0.2 were included in the regression analyses, including in addition province, number of household members, history of chronic liver disease in the family and more than one sexual partner in the last 6 months.
Exposure to HBV (anti-HBc+) was significantly associated (p<0.05) with higher age, living in Bolikhamxay province, living in Pakkading district, not living with parents, not born in Vientiane, higher school grade, a history of chronic liver disease in the family, and lower level of the nearest health care facility (HCF) (Table 11).
In addition, gender, number of household members, history of sexual contact and >1 sexual partner in the past 6 months were associated with exposure to HBV with a p<0.2 and were included in logistic regression analyses.
Table 11. Factors associated with being seroprotected against HBV (anti-HBs+/anti-HBc-) and exposure to HBV (anti-HBc+)
Logistic regression analyses
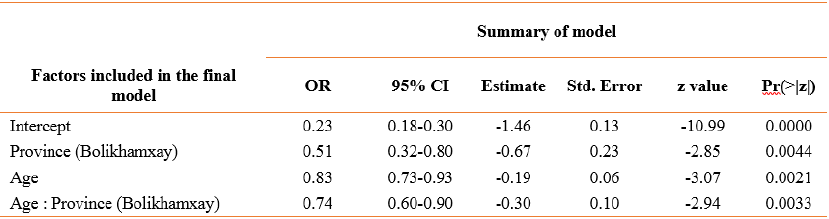
Some variables with low numbers (a living situation, recall of HBV vaccination and the number of sexual partners) were excluded from the multivariable modeling for identifying factors independently associated with vaccination serology. Since a large proportion of the students did not know their place of birth, this variable was also excluded. School grade was excluded since it correlated with age.
Students who were born earlier and recruited in Bolikhamxay were considerably less likely to have a serological profile of vaccination against HBV (interaction term in the model; p=0.003, OR=0.74, CI=0.60–0.90) (Table 12). The overall model was significant (p<0.0001) but the effects of all variables in the final model could only explain 12% of the variability in the dataset (Nagelkerke Pseudo-R2).
Table 12. Binomial generalized linear model showing the factors affecting seroprotection against HBV
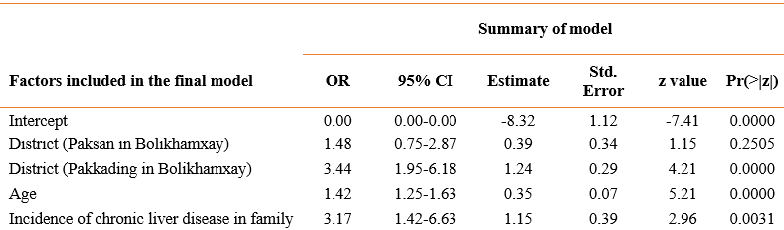
The final multivariable model of risk factors for HBV infection is shown in Table 13. The same variables were excluded for the reasons detailed above. The variables describing province and district also contained the same information and were individually tested in the models. Students living in Pakkading rather than Vientiane Capital (p<0.0001) and older students (i.e. born earlier), as well as students with a known history of chronic liver disease in their families, were more likely to be positive for anti-HBc (p<0.0001 and p=0.003 respectively). The overall model was significant (p<0.0001), but the effects of all variables in the final model could explain only 15% of the variability in the dataset (Nagelkerke Pseudo-R2).
Table 13. Binomial generalized linear model showing the factors associated with being exposed to HBV
Discussion
The proportion of participants with a serological vaccination profile increased only moderately but significantly after the introduction of HBV vaccination into the national vaccination program in both Vientiane Capital and Bolikhamxay province. Logistic regression analyses confirmed that the odds of being protected against HBV through vaccination decreased with age in combination with living in Bolikhamxay province. These results are in line with the somewhat delayed extension of the HBV vaccinations from the Capital to the provinces.
In Bolikhamxay, the vaccination seems to have caught on only in children born and vaccinated in 2004, one year later than in Vientiane. Nevertheless, in both study sites, only about 30% of the participants born 5-6 years (e.g. in 2006-2007) after the introduction of HBV vaccination showed the anti-HBs(+)/anti-HBc(-) vaccination profile, up from pre-introduction levels of 8.3% in Vientiane and 3.3% in Bolikhamxay.
Since this study was done in 2018, more than 10 years after the introduction of the vaccine, these rates reflect vaccine coverage, primary and secondary vaccine failure as well as waning of anti-HBc antibodies after a resolved HBV infection. It is likely that vaccine coverage was initially low and only increased with time to the 85% levels reported in 2017 for the entire country. In addition, in another study, we found that the response to the hepatitis B component of the pentavalent vaccine in children vaccinated with 3 documented doses in 2009-2012 was below 40% within 9-50 months after vaccination, with a considerable waning effect.
In the present study, the relatively modest increase in anti- HBs(+) translated nevertheless into a 2-3 times lower prevalence of markers of resolved (anti-HBc positive) and chronic infection (at least in Bolikhamxay), possibly showing some evidence of less horizontal transmission due to vaccination efforts.
Our findings are comparable to those of other studies observing decreasing anti-HBc positivity rates along with increasing estimated serological vaccination rates after the introduction of HBV vaccination. Furthermore, in logistic regression, older students and students living in Pakkading district, a semi-urban area were significantly more likely to show evidence of past infection with HBV.
However, even among the youngest students between 11- 13 years old, 60% to 75% did not have any serological evidence of successful immunization. However, some of these individuals who may have lost their anti- HBs antibodies despite a previous vaccination may be protected through immune memory. The higher anti- HBc seroprevalence in the older age group may also be partially due to a higher accumulated risk of exposure as the adolescents get older.
Our logistic regression models showed that there were few predictors of past infection or seroprotection against HBV, indicating that there were few systematic risk factors, besides age and location. The relatively low Pseudo-R2 values indicate high variability in the dataset.
Although we can detect these beneficial effects in this early birth cohort, today the seroprevalence of protective anti-HBs antibodies is too low in these adolescents and warrants at least a refresher booster before they enter into a phase of their lives with new risk factors.
Unfortunately, we were not able to assess the association of certain risk factors with the serological profiles due to low numbers. Increased exposure to risk factors for older students may lead to potential health hazards in the future in Lao PDR.
When the serological profiles in 2018 were compared to data from 2011 from Bolikhamxay province, the proportion of students exposed to HBV decreased significantly in the age groups 11 to 14 years, although the prevalence of HBsAg, or chronic infection, did not. This discrepancy may be due to the slow uptake of the birth dose, which even in 2017 was only at 55% nationwide. While the coverage with the pentavalent vaccine (at 6, 10 and 14 weeks) has steadily increased to 85% in 2017 and was effective in reducing infections later in life, it seems to have done little to prevent perinatal vertical transmission and the associated high risk of chronic disease.
Indeed, a history of chronic liver disease in the family was associated with serological evidence of previous infection in our study. These findings underline the importance of further increasing the coverage of the birth dose.
Since we only included students from two provinces, our ability to extrapolate the findings to the whole country is limited. In addition, we only included students from urban and semi-urban areas that belonged mainly to the Tai-Kadai ethnicity. Since vaccination documents for the students in both studies were unavailable to us, we could not interpret the findings with respect to vaccination status or the number of hepatitis B vaccinations. Another limitation of this study is that the risk factor history relied largely on self-reporting.
In conclusion, this study documented a sizable and lasting reduction in past HBV infections in adolescents born early after the introduction of infant HBV vaccination. However, the combination of low coverage and supposedly low immunogenicity resulted in low overall protective levels, which may warrant the introduction of a booster for adolescents at least of these intermediary birth cohorts. Furthermore, additional research may be needed to determine if a booster vaccination is enough to protect these adolescents. A combination of an HBsAg containing vaccine with the planned introduction of the school-based HPV vaccine may be considered. The effect of routine infant vaccination on chronic infection is not measurable, probably because the uptake of the birth dose was very low in these cohorts. There is therefore an urgent need to increase the birth dose coverage significantly higher than the 55% reported in 2017. In addition, awareness campaigns regarding the risk factors of HBV infection should be conducted.
These data were formulated as a policy brief for the relevant partners such as Lao Ministry of Health and were published in the International Journal of Infectious Diseases.