High exposure to hepatitis C virus in Saravan, southern Laos; identification of several risk practices

Participant recruitment, Saravan
VPD laboratory staff; Siriphone Virachith, Vilaysone Khounvisith, Bounta Vongphachanh, Nouna Innoula, Hongnakhone Xayasing, Antony Black.
Collaborating institutions and partners; Centre d’Infectiologie Lao-Christophe Mérieux, Lao Tropical Public Health Institute, Luxembourg Institute of Health. The work was supported by the Fondation Mérieux, Aid Care China and Luxembourg Ministry of Foreign and European Affairs.
Communications; a policy brief was sent to WHO and the Lao Department of Communicable Diseases Control. The data were presented at the Lao Ministry of Health to representatives from WHO, Lao Department for Communicable Disease Control, National Centre for Laboratory and Epidemiology and international organisations. A manuscript has been accepted for publication in Lancet Regional Health: Western Pacific Region.
Background
Our previous hospital-based study in Saravan province, southern Laos, identified a large proportion of individuals who were seropositive for antibodies against the hepatitis C virus (HCV). The majority were from Samuoi district where more than 40% of participants aged over 30 years had anti-HCV antibodies. These data contrasted with the low seroprevalence found in Lao blood donors, female garment factory workers and healthcare workers from other provinces.
With the aim of assessing the risk practices within the community, we returned to Samuoi district from January until March 2022. In order to maximise the number of exposed participants recruited into the study, we selected 24 villages with previously identified seropositive individuals. When possible, these individuals were recruited into the study and age-matched participants (+/- 5 years) were randomly selected from the village name list. All selected participants completed a structured questionnaire to identify risk practices and were then tested for anti-HCV antibodies by rapid test (Standard Diagnostics). Participants were classed as cases if seropositive and controls were seronegative. In the event of newly identified cases, more age-matched individuals were enrolled.
Participants were aged 20 to 90 years and 60.2% were male. There were 160 (39.8%) cases including 18 from the previous study. 94/160 (58.8%) of the cases had detectable viral load (Abbott Real-time HCV assay) and were referred to the district hospital for clinical assessment and treatment (provided by the study).
Overall, there was a high number of reports of having received parenteral medication (58.0%) from nonlicenced practitioners and healthcare workers in public health facilities. Use of re-used syringes was high (72.5% of those that reported receipt of parenteral medication), both by non-licenced practitioners and from the local health care facilities (until 20-25 years ago; personal communication, Dr. Bounluay Suaymanivong, director of the District Health Office; 8 Feb 2022).
Tattooing was frequent (33.1%) and reportedly nonsterile, including sharing of equipment with friends. Piercing was also common (95.0% of women) and nonsterile. Accidental blood exposure was reported by 37.3% of all participants e.g. when helping others who were involved in accidents.
Having tattoos (adjusted odds ratio (aOR), 1.81, 95% confidence intervals (1.2, 2.8), p=0.01) and accidental blood exposure (aOR 1.9 (1.2, 2.9), p<0.01) were significantly associated with anti-HCV seropositivity (Table 1). Viral sequencing is ongoing to determine the epidemiology of the infection in more detail.
This study highlights the urgent need to carry out extensive community-based testing for exposure and ongoing infection and treatment for HCV and possibly also other blood-borne infections in Saravan and also neighbouring provinces in Laos and Vietnam, which might have a similar burden of HCV infection. Community and healthcare worker awareness campaigns are needed, focusing on identified transmission risk practices, how to mitigate them, disease consequences and importance of treatment.
We would like to thank the local healthcare staff, including Bounluay Suaymanivong, Khuanchai Sonkhamphou, Chanthaoudone Chanyaboun and Yup Saypihai, Anouk Neven, participants.
Ethical permission for the study was granted by the Lao National Ethics Committee for Health Research (NECHR#14/2022).
TABLE 1. Characteristics and risk factors of participants.
All data were analysed in R. The adjusted odds ratio for being anti-HCV antibody positive was the main outcome measure. There were no reports of intravenous drug use, dialysis or men who have sex with men.
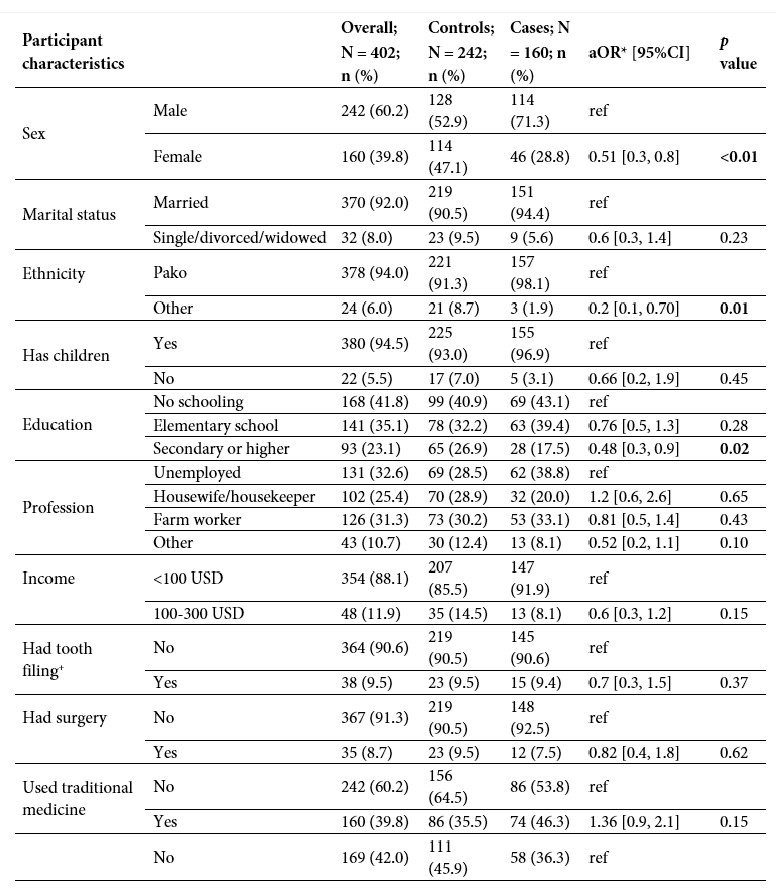
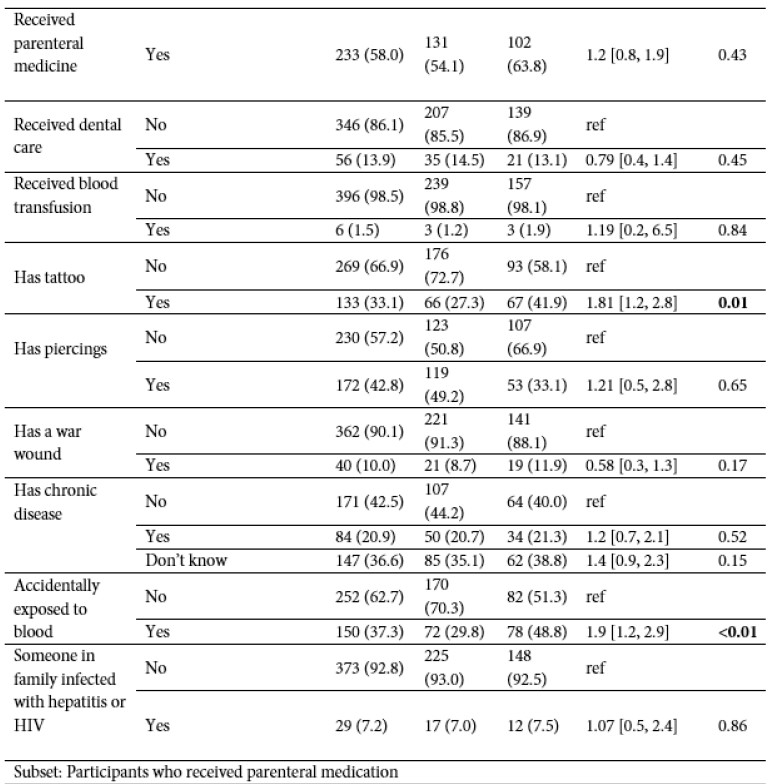
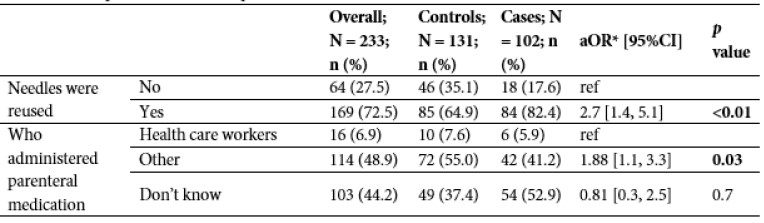
N = total number, n = number, aOR = adjusted odds ratio; 95% CI = 95% confidence interval; USD = United States Dollars
*adjusted for sex and age. No adjustment for multiplicity has been performed. + This traditional practice has largely ceased but, according to the participants, was common among adolescents up until approximately the 1970s.







