Knowledge, attitudes and practices regarding vaccination among healthcare workers in Lao PDR
 Project coordinators: Antony Black
Project coordinators: Antony Black
Staff members: Viengsamay Sengchaleun, Phonepaseuth Khampanisong
Background
Health care workers (HCW) are at increased risk of infection due to vaccine-preventable diseases (VPD) because of their contact with infected patients and contaminated equipment and environments. HCW may also transmit the infection to other staff and patients.
Outbreaks of VPD are common in health-care settings, even in countries with well-established immunization programs. Vaccination of HCW is important to prevent some nosocomial infections.
The World Health Organization recommends HCW should be vaccinated against hepatitis B, polio, diphtheria, measles, rubella, meningococcal, influenza and varicella.
n Lao PDR hepatitis B virus (HBV) infection is endemic; approximately 45% of the general population has been exposed to HBV and 8–10% of the adult population is chronically infected. Outbreaks of other VPD continue to occur due to a combination of low vaccine coverage and poor vaccine immunogenicity. Our previous study found Lao HCW had low levels of protective antibodies against VPD.
Given the low vaccination coverage and rate of people with vaccination-induced protective antibodies among the general population in Lao PDR, HCW vaccination is important. Several knowledge, attitudes and practices (KAP) studies among HCW have been done in the USA, UK and China to evaluate the relationship between knowledge and influenza vaccination.
We aimed to determine the KAP regarding vaccination among HCW in Lao PDR in order to inform VPD control programs to improve the vaccination rate among HCW.
The survey was done on 400 participants from 4 central hospitals in Vientiane Capital (Settathirat, Mitthaphab, Mahosot and Children’s Hospital) and four provincial hospitals (Vientiane, Khammouan, Bolikhamxay and Houaphan). Subjects recruited for the study were physicians (internists, pediatricians, surgeons, obstetricians), midwives, nurses, dentists, lab technicians, administrators and pharmacists.
Results
Socio-demographic characteristics
The mean age (range) of study subjects was 38 (21 to 64) years; 74.7% were female. 40.5% of study subjects were nurses. The mean number of years worked at a hospital was 14. 49.5% of subjects had completed vocational training without further studies (Table 1).
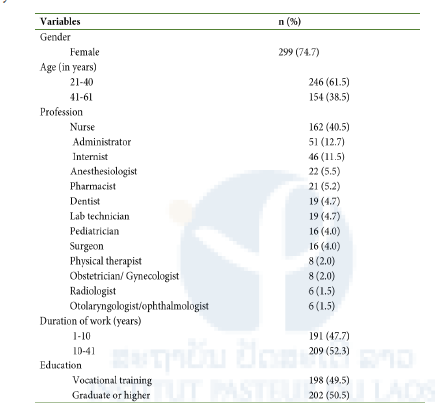
Table 1: Sociodemographic characteristics of study subjects
Knowledge on vaccination
88.7% of study subjects were aware of the existence of an HBV vaccine and 88.2% of the polio vaccines. Eighty-four percent of subjects knew vaccines can have side-effects. 13.5% of subjects believed vaccines can be replaced by traditional medicine. 21.5% of subjects believed a single vaccine dose always provides life-long immunity (Table 2).
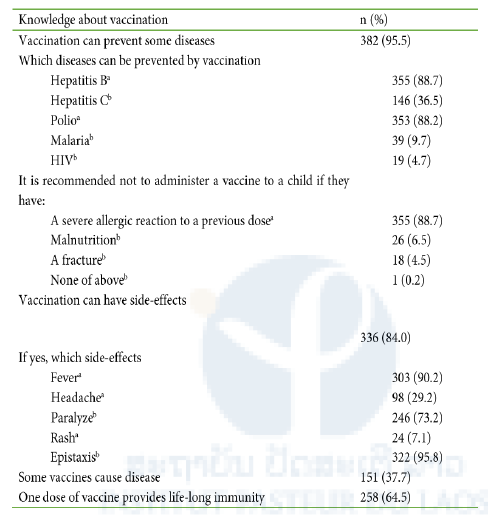
Table 2: Knowledge about vaccination among study subjects
a: correct answer; b: incorrect answer
Awareness of diseases and attitude toward vaccination
Seventy-nine percent of subjects were concerned about contracting a disease while at work; 63.6% of subjects were concerned about contracting HBV infection, 61.0% were concerned about contracting tuberculosis and 56.6% were concerned about contracting HIV infection. 15.5% of subjects were unconcerned about contracting the infection from their patients; of these, 93.5% said they knew how to protect themselves but only 6.5% of them mentioned vaccination as a method of protecting themselves.
Ninety-seven percent of subjects stated HCW should be vaccinated, but only 70.3% stated HCW should be vaccinated against HBV. 86.2% of subjects believed vaccinations were effective in preventing disease, 7.8% were not sure and 6.0% believed vaccinations were not effective in preventing disease; of those, 50.0% stated the reason for this belief was they felt vaccines were not stored correctly. Ninety-five percent of the subjects would recommend vaccinations for their colleagues and 88.2% would recommend vaccinations for their patients. However, only 48.5%of subjects stated they intended to get vaccinations in the future.
Practice
Ninety percent of subjects reported having been vaccinated against at least one disease since starting work in the hospital with the main motivation being self-protection. Among those who had not been vaccinated, the most frequent reason given for not being vaccinated was fear of adverse reactions (Table 3). Of those who had been vaccinated, 73.5% had been vaccinated against HBV. 66.9% of subjects knew their HBV immunity status. Some subjects had been previously vaccinated against poliovirus, tetanus, diphtheria or seasonal influenza; these depended on the availability of vaccines and the presence of epidemics where they lived.
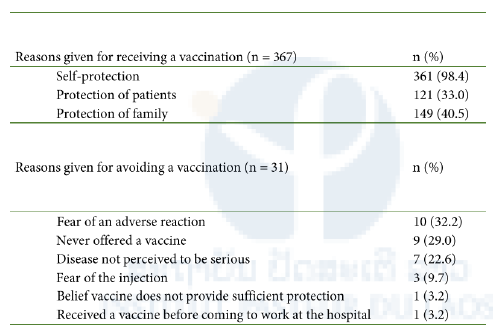
Table 3. Reasons given by study subjects for receiving or avoiding vaccinations.
Information sources and hospital policies
80.5% of study subjects received information about vaccinations from their colleagues and 43.7% received information via their professional studies. 71.7% of study subjects stated their hospitals held information seminars about vaccines and 89.7% stated they always received information from their hospitals during an outbreak.
Eighty-one percent of study subjects stated some vaccinations were provided free at their hospitals, including the influenza vaccine, HBV vaccine, diphtheria vaccine, polio vaccine, tetanus vaccine, measles vaccine, pertussis vaccine, Japanese encephalitis vaccine and rubella vaccine; this varied by the hospital.
Factors associated with a good knowledge about vaccinations after multivariate analysis were: working in a clinical field rather than working in administration (OR: 2.0; 95% CI: 1.2-3.4; p>0.05) and duration of hospital work >10 years (OR: 1.7; 95% CI: 1.1-2.5; p>0.05). Receiving information about vaccinations from colleagues was significantly associated with a favorable attitude toward vaccination (OR: 3.2; 95% CI: 1.4-7.7; p>0.01). Working in a hospital providing free vaccinations was significantly associated with vaccination practice (OR: 3.5; 95% CI: 1.4-8.5; p<0.01). Having a positive attitude about vaccination was significantly associated with practices regarding vaccination (OR: 2.4; 95% CI: 1.1-5.5; p<0.05).
Discussion
The results of this study must be understood in the context of vaccinations among HCW in the Lao PDR. There is currently no national policy in Lao PDR regarding HCW vaccinations, unlike many other countries. A previous study found 53% of HCW in Lao PDR had protective antibodies against HBV infection, the immunity was derived mostly from a previous infection, rather than vaccination. Indeed, only 21% had anti-HBs antibodies without anti-HBc antibodies, indicative of HBV vaccination. Childhood HBV vaccination was only introduced into Lao PDR in 2001.
Vaccination rates among HCW in Lao PDR can be improved by focusing on factors in our study significantly associated with HCW vaccination uptake, such as receiving recommendations by colleagues to be vaccinated and receiving the vaccine for free.
Having a good attitude about vaccination was significantly associated with being vaccinated in our study, similar to a study from Shropshire, United Kingdom that found that the most common reason for being vaccinated against influenza among HCW was believing vaccination to be effective.
A statistically significant association was seen between receiving information from colleagues and being vaccinated. Colleagues played an important role in vaccination decisions. A study from the United States reported the 95% of surveyed parents of children aged ≤18 months accepted advice about vaccination decisions from a “people network” (friend, physician and family). This suggests giving HCW the opportunity to discuss the vaccine with colleagues along with receiving information through seminars that may improve vaccine uptake among HCW. Discussing the potential side effects and benefits of vaccination may also improve uptake among HCW. Misconceptions can also be corrected as seen in study subjects, such as the belief that traditional medicine is as effective in disease prevention as vaccination or a single dose of a vaccine provides life-long protection.
Free vaccination and convenient vaccination should also help improve vaccination uptake by HCW. The hepatitis B vaccine usually costs around 10-20USD per dose in Lao PDR, where many workers received an income of around 200USD per month.
Conclusion
Vaccination is the most effective way to prevent VPD among HCW. Attitudes about vaccination affect vaccination practices. Receiving advice from colleagues and having a free vaccine also improve vaccine uptake. Vaccine promotion programs for HCW should take these factors into consideration. Further studies are needed to determine if the implementation of programs considering these factors can improve VPD morbidity among HCW in Lao PDR. These data have been published as a manuscript in the Southeast Asian Journal of Tropical Medicine and Public Health and were reported as a Masters Thesis for a student from the Lao Tropical and Public Health Institute.







