Evaluation of Insecticide Resistance in Malaria Vectors in the Lao PDR and Thailand (MALVEC)
Supervisors:
1. Paul Brey, Director, Institut Pasteur du Laos, Lao PDR
2. Vincent Corbel, Scientific Coordinator, Institut de Recherche pour le Développement, Thailand
3. Sébastien Marcombe, Project Coordinator, Institut Pasteur du Laos, Lao PDR
4. Hans J. Overgaard, Project Coordinator, Institut de Recherche pour le Développement, Thailand
5. Marc Souris, Representative for Laos and Cambodia Institut de Recherche pour le Développement, Lao PDR
6. Antoine des Graviers, Financial Chief Officer, Institut Pasteur du Laos, Lao PDR
7. Simone Nambanya, Vice Director, Head of Entomology Department, Centre de Malariologie, Parasitologie et Entomologie du Laos, Lao PDR
8. Theeraphap Chareonviriyaphap, medical entomologist head of Entomology Laboratory, Kasetsart University, Thailand

The MALVEC project was held from April 2013 until June 2016. The results and the recommendations that issued from the study were published in a 61-page book which was distributed to the Ministry of Health and the heads of district and provincial health departments countrywide. The book was prefaced by Dr Rabindra R Abeyasinghe, the coordinator of Malaria, Other Vectorborne and Parasitic Diseases for the Western Pacific, at the World Health Organization.
Book publication information
Cover picture

Preface
The malaria burden in the Greater Mekong Sub-region (GMS) remains a major public health problem impacting on the health and lives of a large proportion of people in the GMS countries. This situation has been further complicated by the emergence of falciparum malaria parasites resistant to artemisinin combination therapies (ACTs). The resistance to artemisinin and its partner drugs is a major global health security issue with implications for malaria control efforts not only in the affected countries and the region, but also globally. This will be especially true if resistance were to spread beyond the currently affected countries. In view of this, the WHO has recommended the adoption of a program for the accelerated elimination of malaria from the GMS in 2014 and in 2015 countries of the GMS signed up to a strategy for the elimination of malaria from the GMS.
Malaria control efforts globally and in the GMS have depended largely on the use of insecticide-treated nets and indoor residual spraying. These interventions have contributed to significantly reducing the burden of malaria globally and in the GMS. However, the emergence of insecticide resistance in many malaria-affected countries poses a significant challenge to the continued success of control efforts, including in the GMS countries. Malaria transmission in the Mekong region is currently concentrated in forested and rural areas and along national borders from where the disease is likely to spread to other areas due to the movement of population groups.
The main malaria vectors in the GMS are members of species complexes and accurate identification of vector sibling species, knowledge about their geographic and temporal distribution patterns in countries of the GMS, and understanding their bionomics is important for effective targeting and selection of control interventions. Unfortunately, there are still several gaps in our knowledge of the detailed understanding of the biology of malaria vectors and their role in parasite transmission in the GMS. This project aimed at understanding the distribution of vector sibling species and their ecology and bionomics in the Lao PDR and Thailand. Additionally, the project aimed at understanding the susceptibility status of malaria vectors to insecticides in the project areas in line with recommendations contained in the Global Plan for Insecticide Resistance Management (GPIRM), and aimed at building capacity in entomology in the Lao PDR and Thailand in line with WHO recommendations for scaling up country capacities.
The main malaria vectors in the GMS are members of species complexes and accurate identification o f vector sibling species, knowledge about their geographic and temporal distribution patterns in countries of the GMS, and understanding their bionomics is important for effective targeting and selection of control interventions. Unfortunately, there are still several gaps in our knowledge of the detailed understanding of the biology of malaria vectors and their role in parasite transmission in the GMS. This project aimed at understanding the distribution of vector sibling species and their ecology and bionomics in the Lao PDR and Thailand. Additionally, the project aimed at understanding the susceptibility status of malaria vectors to insecticides in the project areas in line with recommendations contained in the Global Plan for Insecticide Resistance Management (GPIRM), and aimed at building capacity in entomology in the Lao PDR and Thailand in line with WHO recommendations for scaling up country capacities.
Dr Rabindra R. Abeyasinghe
Coordinator,
Malaria, Other Vectorborne and Parasitic Diseases for the Western Pacific,
World Health Organization.
Executive Summary
Insecticide resistance in malaria vectors in South-East Asia represents a serious threat to the achievements obtained in malaria control during recent years. It is important to identify the distribution, levels, mechanisms, and potential environmental factors of resistance in malaria vectors in the lower Mekong countries to assist health authorities to develop effective prevention and control strategies for the disease. Furthermore, there is a general lack of knowledge about the composition, distribution, and host-seeking behavior of Anopheles mosquitoes, especially of sibling species, in the region. Even less is known in malaria hot spots, such as forest areas, and the role of these species in malaria transmission in these areas. In addition, a general lack of expertise in general entomological methods, mosquito identification, insecticide resistance detection, and surveillance further exacerbates the situation.
The MALVEC project, Characterization of insecticide resistance in malaria vectors in the Lao People’s Democratic Republic and Thailand and capacity building in medical entomology, was carried out in the Lao PDR and northeastern Thailand during 2013–2016 with the overall objective to improve strategies for prevention and control of malaria. The specific objectives were to: 1) Evaluate the bionomics and distribution of malaria vectors and their role in malaria transmission; 2) Evaluate the level, type, and mechanisms of insecticide resistance in malaria vectors to conventionally used insecticides; 3) Evaluate the impact of environmental determinants on vector dynamics and insecticide resistance selection; and 4) Build capacity in medical entomology in the Lao PDR and Thailand. As such, the project follows the recommendations of the Global Malaria Action Plan (GMAP) to set up active systems for surveillance of insecticide resistance in vector populations to strengthen the prevention and control strategies against malaria at the global scale. The project was funded by the 5% Initiative of the Global Fund for Malaria, Tuberculosis, and HIV/AIDS and was allocated approximately one million euros over three years.
There was a great abundance and diversity of Anopheles mosquitoes in the study areas with more than 24,000 specimens of at least 27 different species (or species complexes) collected on both human and cow bait in both countries. In addition, molecular identification revealed 13 sibling species within the main primary vector groups (Leucosphyrus, Funestus, and Maculatus groups). Mosquito abundance was much higher in the rainy season than in the dry season. In the Lao PDR, the primary malaria vectors (An. dirus, An. maculatus and An. minimus) were present in all study sites during both the dry and rainy seasons, indicating that people living in these rural areas are constantly exposed to malaria vectors throughout the year. In the Lao PDR, the primary vectors, An. minimus and An. maculatus, were highly zoophilic, but they still bit humans throughout the night with a high peak of activity before midnight, both indoors and outdoors. Overall, 22% of the malaria vectors were collected between 10:00 PM and 5:00 AM indoors when people were sleeping. Although this is a low percentage, it shows the need for the use of bed nets during this period of the night. Twenty-seven percent of primary and secondary vectors were collected outdoors at times when people are usually awake and outdoors (before 10:00PM or after 5:00AM), which shows that people are exposed to potentially infectious mosquitoes and the importance of personal protection at these times. Anopheles dirus is considered as a major malaria vector in the Lao PDR but very few specimens were collected (n=43), which could be explained by its breeding sites usually being located in forested areas and rarely in villages. On the other hand, in the Thai sites along the border with the Lao PDR, there was an extremely low abundance of malaria primary and secondary vectors. However, in forested areas An. dirus was the predominant species biting humans and the human biting rates of this species were more than 30 times higher than in village locations (0.91 vs. 0.03 mosquito bites per person per night). More than 6,400 mosquitoes were tested for Plasmodium presence in both countries and only two specimens were positive; one Anopheles aconitus from Phongsaly Province and one An. minimus from Vientiane Province were infected with P. falciparum, a sporozoite rate of 0.03% (2/6431). Low sporozoite rates are common in the Lao PDR and Thailand, but also reflect the low number of collections (only four nights during the dry and rainy seasons per year) and the very zoophagic and exophagic behaviors of these mosquitoes. This shows again that the transmission may occur outside the villages in forested areas. Additional tools to target outdoor biting mosquitoes are urgently needed for efficient vector control.
Insecticide resistance in malaria vectors in both countries was rare. Only An. maculatus s.l. from Phongsaly and Luang Prabang and An. nivipes from Sekong showed a reduced susceptibility to permethrin. However, reduced susceptibility to DDT was found in several non-vector or secondary vector species (An. vagus, An. philippinensis, An. nivipes, An. kochi, An. tessellatus) throughout the Lao PDR, but also in primary vectors (An. maculatus s.l. and An. minimus in Luang Prabang). These results show that vector control using traditional insecticides is still effective in the Lao PDR, but continued resistance monitoring is necessary to detect potential resistance development at an early stage. Results from Thailand show that the primary vectors are susceptible to all insecticides tested, although sufficient specimens could not be collected for the WHO requirements of complete tests (n>100). Except for a potential resistance in An. barbirostris s.l., all the other secondary vectors were susceptible to pyrethroids and DDT. The only mosquito species with sufficient numbers to make complete bioassays in Thailand was the An. hyrcanus group. All tests indicate a high degree of resistance of this species group to all insecticides tested. No kdr mutation was detected in any of the Anopheles species tested in the two countries, hence suggesting the possible involvement of metabolic resistance. The use of two synergists (PBO and DEF) on the An. hyrcanus group in Thailand strongly increased the efficacy of both permethrin and deltamethrin, hence demonstrating the role of the mono-oxygenases and esterases in pyrethroid resistance. Research on insecticide resistance mechanisms is important to improve the surveillance and management of insecticide resistance and to guide national authorities in vector control policy.
To evaluate the potential impact of environmental factors on vector dynamics and insecticide resistance selection, spatial models were created. These models were based only on environmental, meteorological, and demographic factors and were used to estimate favorable conditions for the presence of malaria vectors and the risk of insecticide resistance in the Lao PDR. A spatial database was built using a GIS (Geographic Information System) to manage and analyze geographic information. The results show that the highest risk of exposure to Anopheles mosquitoes was concentrated in areas in the southern Lao PDR. Insecticide presence and potential selection pressure were also higher in the south of the country, indicating a higher risk of insecticide resistance development. Additional results, such as monthly precipitation, monthly temperature, estimation of monthly mosquito species presence, etc. are available as supplementary material. The results of this work can be used to strengthen public health policies with targeted and effective strategies in the prevention of malaria among populations most at risk, having malaria elimination as a final target. Results may also be used to focus detection of insecticide resistance in Anopheles mosquitoes, reducing considerably the area of surveys and allowing quick deployment of insecticide-resistance management strategies if needed.
Two training sessions were held at Kasetsart University, Bangkok during the project. The first session, Biological methods for detection of insecticide resistance in malaria vectors, was held in November 2013 and consisted of lectures and practical sessions on bioassays, species identification, and mosquito rearing. The second session, Methods for molecular identification of sibling species and Plasmodium detection, was held in October 2014 and contained theoretical lectures and practical sessions on DNA extraction, PCR for sibling species identification, and Plasmodium detection.
Recommendations for Malaria control issued from international experts
At the final MALVEC stakeholder meeting, 21–22 March 2016, in Vientiane, Lao PDR, the participants agreed on the following key recommendations based on the results and outputs of the project. These recommendations are intended for national authorities in order to improve malaria control and accelerate malaria elimination in the Lao PDR
MALVEC RECOMMENDATIONS
+ Achieve universal coverage and proper use of LLIN for people at risk of malaria according to WHO policy and recommendations.
+ Mobilize resources to sustain capacity for insecticide resistance monitoring in the Lao PDR as a basis for insecticide resistance management as outlined in the Global Plan for Insecticide Resistance Monitoring GPIRM (WHO 2012).
+ Mobilize resources to sustain capacity for public health entomology and vector control.
+ Improve the surveillance and stratification methods by using more cost-effective procedures for mosquito collection.
+ Generate complementary data on resistance intensity (and not only the frequency) to measure potential change in the strength of resistance to public health pesticides in malaria vectors.
+ In case of IRS implementation, consider use of non-pyrethroid insecticides to minimize selection pressure on endophagic/endophilic malaria vectors (combination or mosaic strategy).
+ Coordinate action for implementing national registration systems for public health insecticides to avoid the use of illegal products for public health pest and vector control.
+ Investigate the magnitude of malaria transmission (hidden part of the “iceberg”) in hilly, forested areas, rubber plantations, logging camps, etc. by combining entomological, epidemiological, and social surveys.
+ Provide populations at high risk of early/outdoor transmission with more effective tools for personal protection.
+ Mobilize resources for basic research to fill knowledge gaps in the detection of metabolic resistance (e.g. develop PCR tools for tracking resistance markers).
+ Integrate a socio-economic dimension into the fight against malaria as outlined in the Global Malaria Action Plan (RBM 2015).
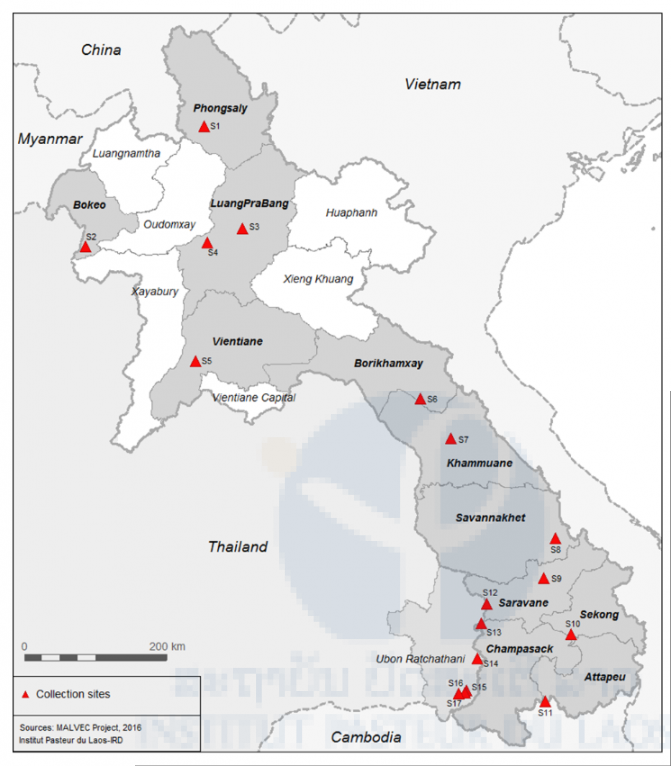
Location of mosquito collection sites during 2013-2015 in Thailand and the Lao PDR
Additional information
Below are some websites with news of and updates on the MALVEC project.
+ Insecticide resistance in malaria vectors in the Lao People’s Democratic Republic and Thailand and capacity building in medical entomology (MALVEC) https://www.pasteur.la/project-carried-on-in-the-lab-5/insecticide-resistance-in-malaria-vectors-in-lao-peoples-democratic-republic-and-thailand-and-capacity-building-in-medical-entomology-malvec/
+ MALVEC project Laos – Evaluation of insecticide resistance in malaria vectors in the Lao PDR and strengthening capacity in medical entomology [in French] http://www.laos.ird.fr/les-activites-scientifiques/projets-de-recherche/projet-malvec-laos
+ Medical entomology training for Lao and Thai partners 11 November 2014 http://www.thailand.ird.fr/all-the-news/news/medical-entomology-training-for-lao-and-thai-partners
+ MALVEC Project dashboard available at http://www.malvec.pasteur.la and http://www.malvec.ird.fr
http://www.initiative5pour100.fr/qui-sommes-nous/actualite-archives/page/3/

https://www.expertisefrance.fr/documents/20182/426622

Publications
Marcombe S, Bobichon J, Somphong B, Phommavan N, Maithaviphet S, Nambanya S, Corbel V, and Brey PT. Insecticide resistance status of malaria vectors in the Lao PDR. 2017. PloS One 12 (4).
Souris M, Marcombe S, Laforet J, Brey PT, Corbel V, and Overgaard HJ. Modeling spatial variation in risk of presence and insecticide resistance for malaria vectors in Laos. 2017. PloS One 12 (5).
Sumarnrote A, Overgaard HJ, Marasri N, Fustec B, Thanispong K, Chareonviriyaphap T, and Corbel V. 2017. Status of insecticide resistance in Anopheles mosquitoes in Ubon Ratchathani province, Northeastern Thailand. Malaria Journal, 16, 299. http://doi.org/10.1186/s12936-017-1948-z
Marcombe S, Bobichon J, Somphong B, Phommavan N, Maithaviphet S, Nanbanya S, Corbel V, and Brey PT. Bionomics, diversity and distribution of Anopheles mosquitoes in the Lao PDR. In progress.
Marasri N, Overgaard HJ, Sumarnrote A, Thanispong K, Corbel V, and Chareonviriyaphap T. Diversity, distribution and behavior of Anopheles mosquitoes along the Thai–Lao border, Ubon Ratchathani province, northeastern Thailand. In progress.
Overgaard HJ, Celhay O, Sumarnrote A, Marasri N, Chareonviriyaphap T, Thanispong K, and Corbel V. Malaria in Ubon Ratchathani province, northeastern Thailand. In progress
Sumarnrote A, Overgaard HJ, Thanispong K, Corbel V, Chareonviriyaphap T, and Manguin S. Molecular identification of species in the An. hyrcanus Group in Thailand. In progress.







